What Is an Emergency Room Doctor?
An emergency room doctor, or “ER doctor,” typically works in an emergency department in a hospital or an urgent care facility. The doctor’s main job is to stabilize a patient. After the patient becomes stable, the doctor can pinpoint the source of the injury and begin the treatment process.
An ER doctor treats various issues, from acute medical problems to larger traumatic injuries. The ER doctor makes the final call on whether or not the emergency treatment is sufficient for the injury at hand or if further appointments should be made with specialists.
The scope of treatment an emergency medical doctor provides is vast. Their demographics include women and children of any age with illnesses at every stage of severity and progression. An ER doctor will be very familiar with treating issues in pulmonology, cardiology, neurology, dermatology, psychiatry, and many others. Typically their job is to assess the injury or illness to produce one of two outcomes.
With smaller, less serious cases, they will treat a patient and discharge them. In more serious, chronic situations, the ER doctor will refer a patient to a specialist for more in-depth, long-term treatment. In the most severe cases of trauma, such as heart attack, stroke, or other life-threatening injuries, an emergency room doctor will begin treatment instantly. Life-or-death situations present themselves to doctors in emergency units on a daily basis. An ER doctor often finds themselves as the only doctor present on a shift in an emergency unit. These situations can be very hectic. It is very important that the doctor is able to quickly triage patients and separate cases based on severity.
The most life-threatening cases will be a top priority. Patients are triaged and seen in an order based on the importance of the medical emergency. If you’ve ever experienced a long wait in an urgent care facility or hospital emergency room, chances are your illness or injury wasn’t as serious as others patients that may have been seen before you.
Different Types of Emergency Doctors
Normally ER doctors are the most common types of practicing physicians in the category of emergency medicine. However, there are normally two distinct positions available for practicing physicians that enter the field of emergency medicine. One example is an orthopedic trauma surgeon. There are several different types of trauma surgeons. Let’s examine the differences between the position of trauma surgeon and actual ER doctor.
Difference in Skills and Job Demands
ER Doctor
Although the goals for the end result of a patient are the same when it comes to a trauma surgeon and ER doctor, the job description separates them. These jobs require two entirely different skill sets. An ER doctor will visit each and every patient who walks through the doors of an emergency room or urgent care facility. Regardless of the injury, each patient will be seen at some point by the ER doctor in order to classify them and determine the best course of treatment.
In cases of severe trauma, an ER doctor will intubate a patient, begin blood transfusions, or order rounds of testing. The ER doctors job is to stabilize a patient.
Trauma Surgeon
A trauma surgeon typically is not stationed in the emergency room at all times. If patients fall into certain emergency categories, a trauma surgeon will be called in to perform an emergency procedure. Some of the situations that require a trauma surgeon may include:
- Low blood pressure after trauma
- Gunshot wounds
- Imaplement and severe lacerations
If a patient enters the emergency room and the extent of the injuries are already known to be quite severe, the trauma surgeon may join the ER doctor from the start of the treatment. If a patient is admitted for their trauma and surgery is required, the trauma surgeon becomes their primary care provider for the visit. They will assume all care and order return visits if they are required.
Differences in Educational Demands
ER doctors and surgeons undergo the same level of education throughout their college careers. The two will follow the same path through medical school until they graduate. The differences in training do not arrive until after they graduate. Upon entering their residency, the two will take a completely different path regarding their hands-on training. An ER doctor will undergo a three or four-year residency program. Upon completion, they will typically be ready to enter the work field.
The demands for a trauma surgeon are much higher. Any surgeon will undergo a five—or six-year residency regardless of the type of surgery they decide to specialize in. Surgeons electing to specialize in trauma will incur an additional one or two years of critical care and trauma training.
Contact and Journey With Patients
Another critical difference in the job description is the contact an ER doctor or trauma surgeon will have with patients. Normally an ER doctor will see the patient during the initial emergency room visit. Upon their discharge or transfer, the ER doctor’s interaction with that patient is over.
A trauma surgeon often completes a much longer journey with each respective patient. A trauma surgeon will often follow a patient well after the surgical process. It is not uncommon for a trauma surgeon to continue interacting with a patient all the way through the rehabilitation process.
Practice Opportunities for an ER Doctor
Once a student receives their degree and completes their residency, several practice model options are available. At this stage, an emergency doctor will decide what type of organization they will work for.
A doctor can decide to work for three main types of organizations.
- Private group
- Corporate group
- Hospital
Private or Democratic Group
Many private groups offer the potential for a long-term partnership for a doctor. This means that eventually, a doctor could become part owner of the practice. Other types of organizations offer the option for financial equity and the ability to make important decisions in the practice’s interest.
A private group is also known as a democratic group. Doctors can have a major voice in the organization and receive a vote when it comes to major decisions. With ownership as an option in a democratic group, a doctor can benefit from the organization’s success. Democratic organizations often have the highest compensation and profit available for doctors.
Corporate Group
Different medical organizations tend to overlap. Corporate groups are sometimes seen as democratic or private groups due to the fact that they are often owned by physicians or a group of physicians. The major difference between the two is normally the size of the emergency departments the two operate. While a private or democratic group would normally operate several emergency departments (upwards of 10), a corporate would typically only be responsible for one or two.
Hospitals
The amount of hospital employees has been on an upward trend in recent years. Doctors who work as employees in a hospital setting have varying degrees of political and financial equity depending on the situation. Hospital positions normally share characteristics that are more similar to those of a corporate group. A doctor normally will see his or her position and authority rise with their years employed by the hospital.
One bonus included with a hospital position is job security. Hospitals normally want to avoid situations of liability or wrongful termination, leading to a more secure position by an emergency room doctor. It is often much easier for a board of directors in a corporate group to make the decision to remove a doctor from the schedule than it would be for a hospital to terminate a physician completely.
The type of organization a doctor works for is one of the most important decisions they will face while starting their career. It is important to consider your future and what path you see yourself on before making a final choice on the type of organization to join. Our pre-med advisors can provide you with more information pertaining to this category. Internship programs may offer information to help you decide on what organization is best to strive towards.

How to Become an Emergency Room Doctor
In the next section, we will examine the steps required in college to become an ER doctor. Read on as we break down in depth what you can expect from each school year on the journey to receiving your degree.
Earn Your Bachelors Degree
Freshman Year
- Health Care Systems
- Biology 1
- Biology 2
- Calculus 1
- Chemistry 1
- Chemistry 2
- Humanities Requirement
- Electives
Sophomore Year
- Public Health
- Anatomy and Physiology 1
- Anatomy and Physiology 2
- Statistics
- Organic Chemistry 1
- Organic Chemistry 2
- Basic Skills for Healthcare
- Nutrition
- Humanities Requirements
- Electives
Junior Year
- Healthcare Communication
- Healthcare Professional Writing
- Genetics and Microbiology 1
- Physics 1
- Physics 2
- Problems in Healthcare
- Healthcare Research
- Biochemistry 1
- Humanities Requirements
- Electives
Senior Year
- Health in the U.S.
- Health Education and Planning
- Healthcare Management
- Health Policy
- Capstone
- Remaining Electives
Take the Medical College Admissions Test (MCAT)
Biology and Chemical Foundations of Living Systems
- 59 questions (multiple choice)
- 95 minutes allowed
- Tests for biology, organic chemistry, inorganic chemistry, and biochemistry
Chemical and Physical Foundations of Biological Systems
- 59 questions (multiple choice)
- 95 minutes allowed
- Tests for biochemistry, biology, general chemistry, organic chemistry, and physics
Psychological, Social, and Biological Foundations of Behavior
- 59 questions (multiple choice)
- 95 minutes allowed
- Tests for introductory psychology, sociology, and biology
Critical Analysis and Reasoning Skills
- 52 questions (multiple choice)
- 90 minutes allowed
- Tests for reading comprehension, humanities, and social sciences
Earn a Medical Degree (4 Years)
Medical school consists of four years of studying the basics of science and participating in clinical rotations. These are real hands-on clinicals that take place in a legitimate healthcare setting.
Year 1
- Cells and Tissues
- Molecular Foundations of Medicine
- Applied Biochemistry
- Genetics
- Disease Mechanisms and Development
- Cardiac Life Support
- The Nervous System
- Immunology
- Gross Anatomy of Head and Neck
- Microbiology
- Pulmonary Systems
- Microbiology
Year 2
- Renal/Genitourinary Systems
- Gastrointestinal Systems
- Skin/Endocrine Systems
- Reproduction and Women’s Health
- Microbiology
- Behavior and the Brain
- Hematology
- Systemic Diseases
- Microbiology
- Clinical Clerkship
Year 3 and 4
- Internal Medicine
- Pediatrics
- Surgery
- Obstetrics and Gynecology
- Family Medicine
- Psychiatry
- Neurology
- Critical Care
- Ambulatory Medicine
- Research, Reflections, and Advances in Patient Care
Pass the United States Medical Licensing Exam (USMLE)
Every state requires a physician to pass a standardized exam. Requirements may vary from state to state. All potential ER doctors must pass the USMLE exam. The USMLE exam is sponsored by the National Board of Medical Examiners (NBME).
Complete a Three to Four Year Residency
An ER doctor’s residency must be completed in a facility that is approved by the Residency Review Committee.
There are over 9,400 graduate medical education programs in the United States. The field is highly competitive, and acceptance is based on academic performance and recommendations by medical school professors.
Earn an Emergency Medicine Certification
Once a residency is completed, the Emergency Medicine Certification is obtained by completing a written and oral exam. Every ten years, recertification is required to continue holding the certification.
Emergency Room Doctor Extra Requirements
Depending on whether or not a doctor decides to take up a specialty sector of emergency medicine, there may be continuing education required. Different boards are included in special categories of emergency medicine, such as the American Osteopathic Board of Emergency Medicine and the American Board of Medical Specialties, that require maintenance board certification.
Most medical schools offer a continuing education department in departments such as emergency medicine that offer courses based on this model.
Fellowships may be required if an ER doctor takes up a special branch of emergency medicine, such as medical toxicology, pediatric emergency medicine, or sports medicine. These also carry specialty board certifications and maintenance requirements.
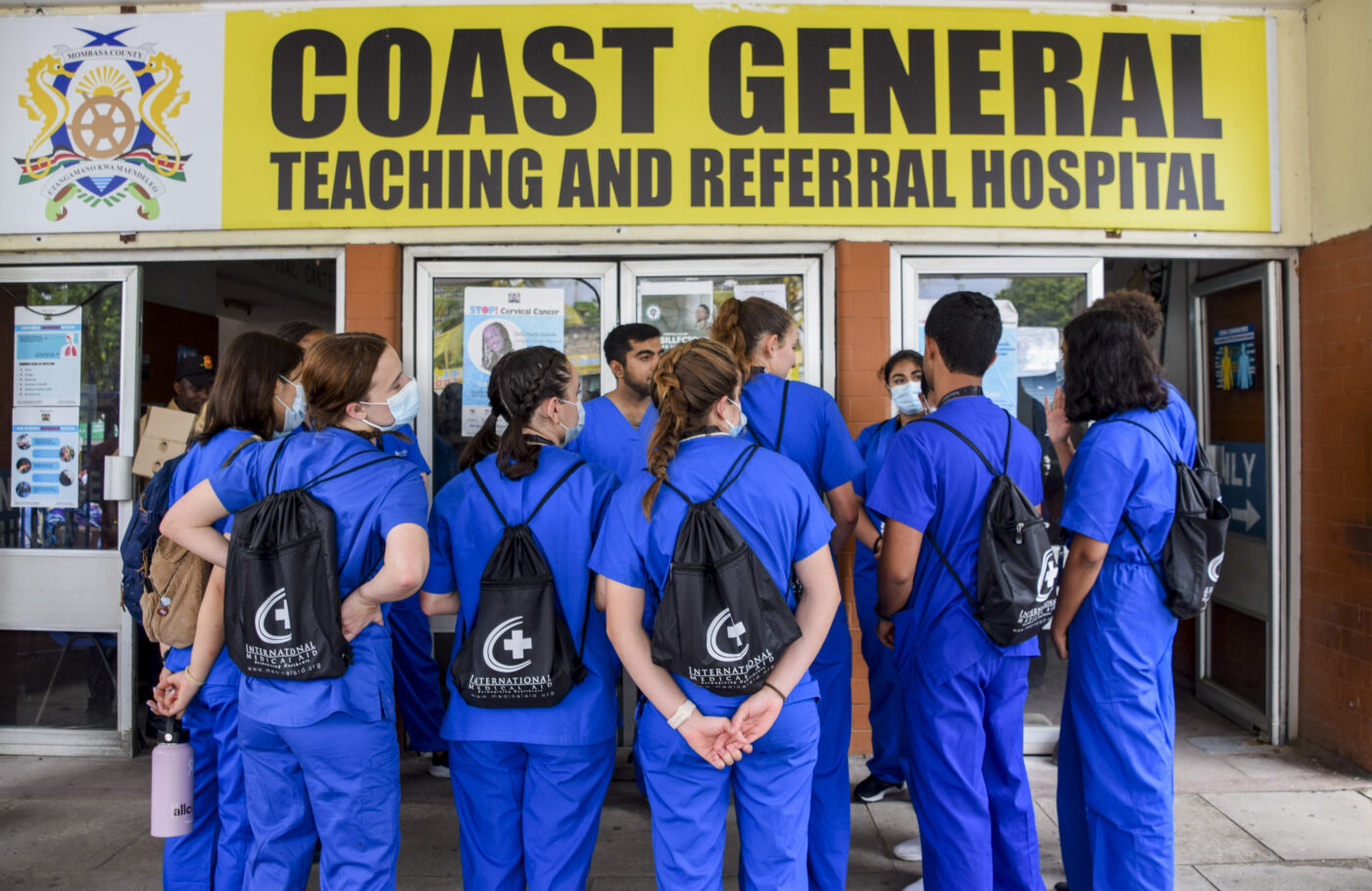
Added Benefits/Opportunities
Another added benefit to becoming an ER doctor is the ability to travel. For the adventurer or roaming type, there are many different opportunities to study and work abroad in many different countries. There is a constant need for medical expertise in countries where advancements and certified doctors are not abundant. This can be exciting and very fulfilling in the sense that you get to travel and help people in need. Our website contains an extensive section about traveling, studying abroad, and working in other countries.
Innovations in Emergency Medicine
Digital Transformation in the ER
Emergency departments have evolved into technology-driven environments. The rapid integration of digital triage systems, real‑time patient monitoring, and telemedicine platforms has transformed how emergency care is delivered. Modern ER doctors now have immediate access to comprehensive patient data and automated decision‑support tools that help speed up critical diagnoses. These digital advancements enhance the accuracy of treatments and allow physicians to collaborate seamlessly with remote specialists, ensuring that even in high-pressure situations, every patient receives a tailored, evidence‑based approach to care.
The Impact of Technology on Triage
One of the most significant developments in recent years is the implementation of artificial intelligence in patient triage. AI algorithms now help ER doctors rapidly analyze patient data—from vital signs to imaging results—predicting the severity of conditions with remarkable accuracy. This technology augments the physician’s expertise, allowing for a more efficient sorting of cases and ensuring that life‑threatening conditions are identified and treated without delay. The AI‑assisted triage process also alleviates some of the workload during peak times, enabling ER teams to focus on delivering hands‑on care where needed most.
Evolving Training and Education for Emergency Medicine
Simulation‑Based Learning in Clinical Training
As emergency medicine becomes increasingly complex, simulation‑based learning has emerged as a critical component in medical training. Modern simulation labs offer realistic, immersive environments where future ER doctors can practice critical procedures—from intubations to advanced cardiac life support—without risk to real patients. These simulations and debriefing sessions provide invaluable feedback and help trainees build confidence and sharpen their clinical decision‑making skills. The hands‑on experience gained through simulation training is now an integral part of residency programs, ensuring that new doctors are well‑prepared for the unpredictable challenges of the emergency department.
Interdisciplinary Collaboration and Continuous Education
Modern emergency medicine demands a collaborative approach to patient care. Training programs now emphasize interdisciplinary learning, encouraging ER doctors, trauma surgeons, and other specialists to work closely together from early in their careers. This collaborative model strengthens team dynamics and facilitates the exchange of ideas and best practices, ultimately leading to improved patient outcomes. Continuous education through online platforms and virtual conferences ensures that even seasoned professionals stay updated on the latest techniques and innovations in emergency care. These digital learning tools are reshaping how ER doctors maintain their skills and adapt to new clinical challenges.
Global Perspectives in Emergency Care as an Emergency Room Doctor
International Exchange and Best Practices
Exposure to international healthcare systems is becoming a cornerstone of advanced emergency medicine training. Many ER doctors are now participating in exchange programs and global health initiatives that broaden their perspective on patient care. By learning from diverse healthcare environments—ranging from resource‑limited settings to state‑of‑the‑art hospitals—doctors acquire unique insights into innovative treatment protocols and cost‑effective care strategies. This global exposure not only enriches their professional development but also inspires the implementation of successful practices in their own communities, contributing to overall improvements in emergency care.
Cultural Competence and Patient Communication
As patient populations become more diverse, cultural competence has emerged as an essential skill for ER doctors. In international settings, understanding cultural nuances can be the key to effective communication, helping physicians navigate language barriers and build trust with patients from various backgrounds. This focus on cultural sensitivity ensures that emergency care is respectful and effective, ultimately leading to better patient satisfaction and improved health outcomes. By embracing these global perspectives, ER doctors are better equipped to provide individualized care that respects every patient’s unique needs and values.
Complete Source List
- Bureau of Labor Statistics. “Occupational Outlook Handbook: Physicians.” https://www.bls.gov/ooh/healthcare/physicians-and-surgeons.htm
- American College of Emergency Physicians. “Advances in Emergency Medicine.” https://www.acep.org/
- National Institutes of Health. “Telemedicine and Digital Health in 2025.” https://www.nih.gov/
- Journal of Emergency Medicine. “The Impact of AI on Patient Triage.” https://www.jem-journal.com/
- American Medical Informatics Association. “Digital Innovations in Healthcare.” https://amia.org/
- International Medical Aid. “Nursing/Pre-Nursing Internships Abroad.” https://medicalaid.org/internships/pre-nursing-nursing-internship/
- International Medical Aid. “How Nursing Internships Shape Future Caregivers.” https://medicalaid.org/how-nursing-internships-shape-future-caregivers/
Conclusion
Becoming an ER doctor requires extreme dedication, a love for your craft, and a leap of faith. Every decision you make along the way will have lifelong repercussions. Rarely do future doctors make these decisions alone.
We strongly advise against making these vital decisions without some sort of guidance. With some type of guidance, the chances of you sticking to the decisions you make for the long haul increase drastically.
We offer several programs for future doctors to help them along the way. In addition to mentoring and studying abroad, we also offer several different internships.
We invite you to read up on and apply to our healthcare internship program. At International Medical Aid we are confident that we can help you achieve your goals with our mentorship experts. Let us help you walk the right path!