The path to medical school is lined with numerous challenges and hurdles, with perhaps one of the most daunting being the Multiple Mini Interview (MMI). As part of the medical school admissions process, the MMI stands as a unique opportunity for applicants to demonstrate not just their knowledge, but also their communication skills, ethical reasoning, empathy, and more. This extensive guide is designed to demystify the MMI process, providing a comprehensive guide filled with practice MMI questions, expert responses, and invaluable tips.
What Are MMI Interviews?
The MMI, or Multiple Mini Interview, is a series of short, structured interviews used by medical schools to evaluate a candidate’s soft skills. Initially developed by McMaster University, it has been adopted by numerous medical schools near me and around the world. Unlike traditional interviews, MMI does not focus exclusively on academic achievements or knowledge. Instead, it assesses an applicant’s communication skills, ethical judgement, critical thinking, and ability to handle stressful situations — all key qualities of a competent healthcare professional.
In an MMI, applicants rotate through multiple stations (typically 6-10), each presenting a different scenario or question. At each station, they have a brief amount of time (usually 2 minutes) to read the scenario and think about their response. They then have around 5-8 minutes to respond or interact with an interviewer or actor.
Preparing for Your MMI Interview
The Multiple Mini Interview (MMI) format might seem intimidating due to its unique structure and wide-ranging question types. However, with the right preparation and mindset, it’s possible to tackle this effectively and leave a lasting impression.
Understand the MMI Process
First and foremost, gaining a thorough understanding of the MMI format is crucial. This includes knowing how many stations to expect, the time allocated per station, and the rest period between each. You should also familiarize yourself with the different types of MMI stations, such as scenario-based questions, traditional interview questions, role-play scenarios, and collaborative tasks.
Additionally, take the time to research the specific nuances of the institution where you are interviewing. While the general format of the MMI remains constant, individual schools might have unique elements in their interview process.
Reflect on Your Experiences
The MMI is designed to assess a candidate’s non-cognitive skills, such as empathy, ethical decision-making, and communication. To prepare for this, reflect on your past experiences, both personal and professional, which have shaped these skills. This could include experiences with teamwork, leadership, conflict resolution, and instances where you’ve displayed resilience or adaptability.
Remember, the goal is not to regurgitate pre-rehearsed answers but to provide sincere, thoughtful responses. Interviewers are looking for insight into your thought process, values, and character, so make sure your answers reflect that.
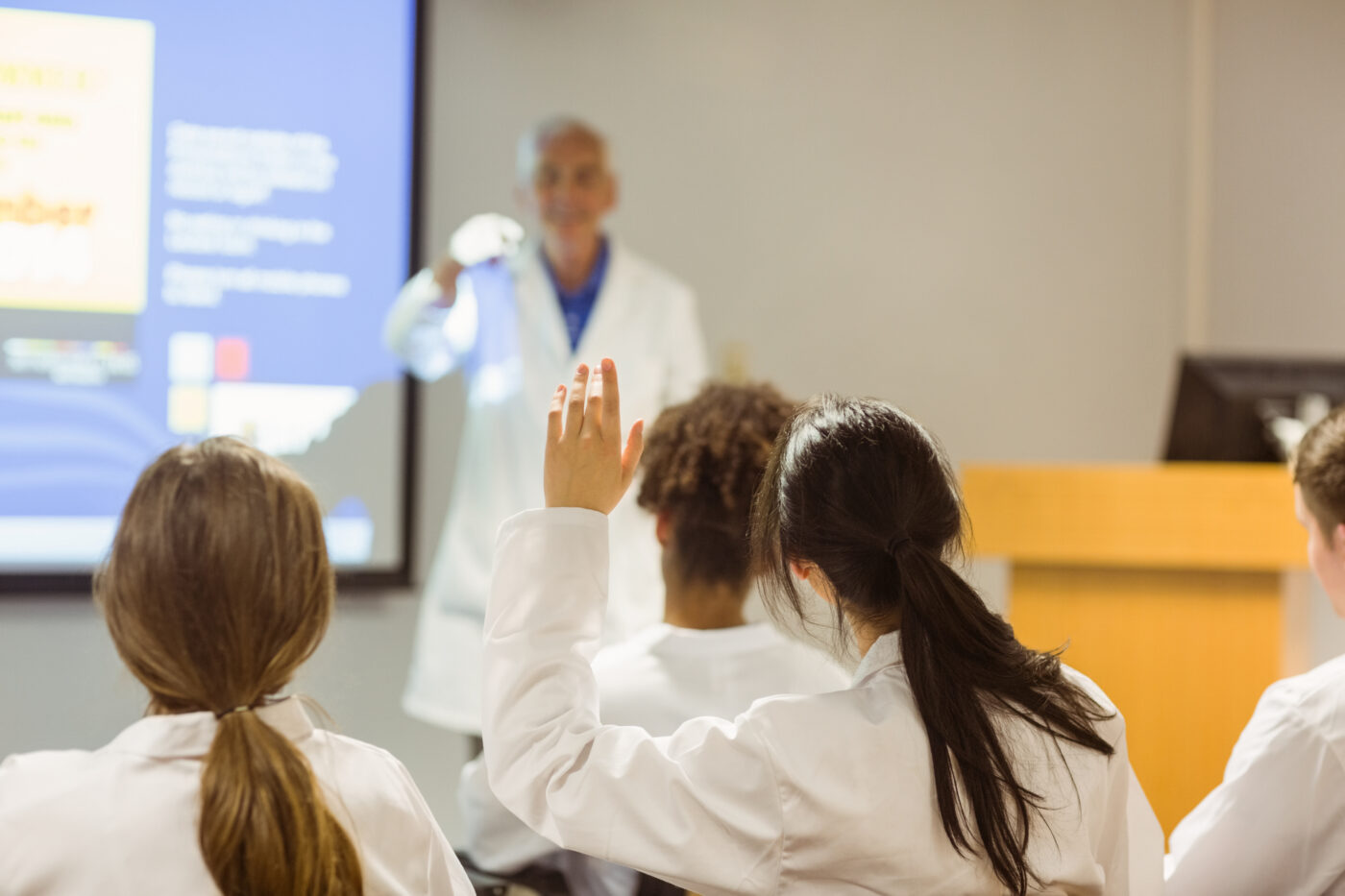
Practice Under Similar Conditions with IMA's Admissions Consulting Program
Practicing under conditions similar to an MMI is essential, and this is where International Medical Aid’s Medical School Admissions Consulting program truly shines. The program offers comprehensive MMI interview preparation, which includes providing a wealth of MMI questions and scenarios to practice with. Their expert consultants will replicate the timing and structure of an MMI interview, allowing you to get comfortable with the pace and variety of questions that you will encounter.
Moreover, with IMA’s admissions consulting program, you will receive personalized feedback on your responses. This can give you unique insights into your strengths and areas for improvement, helping you hone your communication skills, ethical reasoning, and overall approach to MMI questions.
So, in your MMI preparation journey, consider using IMA’s Medical School Admissions Consulting program. It is designed to provide the guidance, practice, and feedback needed to help you perform at your best during your MMI interview.
Rely on International Medical Aid's School Admissions Consulting
Making the most of a specialized service like International Medical Aid’s Medical School Admissions Consulting can significantly boost your MMI preparation. Our consultants are seasoned professionals who have a nuanced understanding of the MMI process, and they are equipped to provide specific, detailed feedback on your responses. They’ll assist you in recognizing areas for improvement and furnish guidance on the optimal ways to articulate your thoughts and ideas.
More than that, we at International Medical Aid go the extra mile to simulate the MMI conditions accurately, affording you a firsthand experience of the interview format. This comprehensive service helps you get comfortable with the MMI and prepares you to handle it with confidence.
In the end, successful MMI preparation hinges on thoughtful self-reflection, thorough practice, and a deep comprehension of the process. When you leverage the right resources like International Medical Aid’s Medical School Admissions Consulting and undertake diligent preparation, you’re setting yourself up to adeptly manage any MMI scenario thrown at you.
MMI Interview Question Categories
MMI interview questions can be categorized into several types. Understanding these categories can help you predict the kind of skills each question is designed to assess and prepare accordingly. Here are some common categories:
- Ethical Decision-Making: These questions focus on your ability to understand, analyze, and resolve ethical dilemmas in healthcare. They test your moral judgement and ability to navigate complex situations.
- Critical Thinking: This category assesses your problem-solving skills, analytical thinking, and decision-making process. Questions might involve interpreting data or proposing solutions to complex healthcare issues.
- Communication Skills: These questions are designed to gauge your ability to communicate effectively with patients, families, and healthcare teams. They may include tasks such as explaining a diagnosis or plan of care.
- Teamwork and Collaboration: Some stations involve multiple candidates or actors and are designed to assess your teamwork, leadership, and conflict resolution skills.
- Empathy and Compassion: Questions in this category evaluate your ability to show empathy, kindness, and understanding towards patients’ experiences and emotions.
- Cultural Competence: This category includes questions about dealing with diverse patient populations, addressing disparities in healthcare, and respecting cultural differences in healthcare contexts.
- Personal Experiences: These questions seek to understand your personal experiences, motivations for pursuing medicine, and reactions to certain situations.
- Healthcare and Policy Knowledge: These questions focus on your understanding of current health policy, medical ethics, and major issues in healthcare.
- Role Play: Role-play stations involve interactions with actors playing patients, family members, or colleagues and are designed to evaluate your communication, empathy, and problem-solving skills.
- Scenario-Based Questions: These questions present a scenario or task that you have to deal with, such as breaking bad news to a patient or resolving a conflict.
Each of these categories assesses different aspects of your character, skills, and suitability for the profession. Admissions consulting, like the services offered by International Medical Aid, can provide specific strategies for dealing with each type of question.
MMI Sample Questions and Expert Responses
In this section, we will present 200 sample MMI questions, divided according to the categories mentioned earlier. Each question will be accompanied by an a few expert responses that demonstrate the desired skills and reasoning. Keep in mind that these responses are not scripts to memorize, but examples of how you might structure your answers. Each scenario should be approached with authenticity and personal insight.
Let’s start with the first category, Ethical dilemmas.
Ethical Decision-Making
Questions in this category assess your understanding of ethics and your ability to navigate complex moral situations. They typically present hypothetical or real-life dilemmas and ask you to discuss or resolve the issue, showcasing your ethical judgment.
Question 1: A patient with a terminal illness asks you to help them end their life. How would you handle this situation?
Expert Response: The topic in question is indeed complex and ethically challenging. My empathy extends to the patient’s plight, yet my role as a medical professional emphasizes life preservation and comfort provision to the utmost of my capabilities. Assisting in terminating a life opposes these obligations. I would engage the patient in a conversation regarding their feelings, fears, and concerns, while ensuring they have access to optimal palliative care for symptom and pain management.
Question 2: You are a medical student observing a surgery and you notice that the surgeon has made a mistake. The surgeon has not noticed the mistake. What do you do?
Expert Response: In my capacity as a medical student, my procedural comprehension is more limited than a qualified surgeon’s. Nonetheless, patient safety remains paramount. I would convey my concerns to the surgeon, ensuring this conversation happens in a respectful and private manner. Clear and open communication is vital in the interest of patient care.
Question 3: You have a patient who needs a blood transfusion to live, but they are a Jehovah's Witness and their religion prohibits receiving blood products. What do you do?
Expert Response: Respecting patient autonomy and religious beliefs is imperative. I would have a transparent discussion with the patient or their representative, laying out the situation and consequences of not proceeding with the transfusion. I would also investigate alternative treatments that are in line with their faith, and seek advice from my peers and the hospital’s ethics committee.
Question 4: You are a pediatrician, and a child's parents refuse to have him vaccinated. How do you respond?
Expert Response: Vaccines play a critical role in protecting both individuals and public health. However, this situation raises the issue of parental rights and possibly differing beliefs. I’d first make sure the parents have accurate, evidence-based information about the advantages and risks associated with vaccinations, addressing any misconceptions they might have. Should they persist in their refusal, I would respect their decision, but emphasize the potential health risks to their child and the wider community.
Question 5: A patient has been pronounced brain dead, and their family is in denial. How do you handle this situation?
Expert Response: I would approach this scenario with understanding, empathy, and patience, taking the time to explain the medical definition of brain death and its irreversible nature. It’s crucial to offer them time to process the information and provide access to counselling resources. Even under these difficult circumstances, maintaining sensitivity and respect for the family’s emotional state remains paramount.
Question 6: Imagine a parent doesn't want to inform their child about a grave diagnosis. How would you navigate this delicate situation?
Expert Response: In such a situation, it’s vital to respect the parents’ wishes while also considering the child’s right to know. I would initiate a discussion with the parents, seeking to understand their concerns and providing advice on the potential benefits of honesty. If possible, we would work together to find an appropriate way to communicate the situation to the child.
Question 7: Suppose you're an OB/GYN. One of your pregnant patients is considering a strict diet that might harm her unborn baby. What steps do you take?
Expert Response: Patient safety is always a priority, especially in prenatal care. I would discuss the potential risks of the strict diet to both the patient and her unborn baby. I would also explore with her the reasons behind this decision, aiming to provide suitable alternatives and nutritional guidance that would not compromise her or her baby’s health.
Question 8: You spot odd behavior in a colleague that makes you suspect substance abuse during work hours. What's your course of action?
Expert Response: Patient safety and professional ethics would guide my actions in this scenario. It’s crucial to approach the situation delicately. I’d initiate a private, non-confrontational conversation with my colleague about my observations. If the behavior continues or if patients are at immediate risk, I would report the situation to a supervisor.
Question 9: Let's say you're a general practitioner. A close friend, who is also your patient, wants a medical certificate from you, claiming they're unfit to work when they're not actually sick. How do you manage this?
Expert Response: While it’s important to maintain trust in personal relationships, professional integrity comes first. I would discuss the implications of false documentation with my friend, emphasizing that it’s unethical and can undermine trust. I’d suggest discussing their work concerns honestly with their employer instead.
Question 10: Imagine you're a surgeon who has committed an avoidable error during a procedure. The patient is unaware of it so far. What steps do you take?
Expert Response: Mistakes are difficult to accept, especially when they may impact patient health. However, transparency and honesty are integral to healthcare. I would notify my immediate superior about the situation, take necessary remedial actions, and disclose the error to the patient while explaining the steps taken to address it.
Question 11: A patient with a critical illness is eager to try an experimental treatment you're convinced won't be effective. How do you address this?
Expert Response: It’s important to support a patient’s hope while providing medical facts. I’d thoroughly discuss the pros and cons of the experimental treatment, ensuring the patient understands its experimental nature and potential inefficacy. I would also discuss other available treatments and seek a consensus on the best way forward.
Question 12: A necessary procedure is being refused by your patient due to fear. What is your response?
Expert Response: Fear and anxiety are common responses to medical procedures. In this case, I would take time to address my patient’s fears, explaining the procedure, its necessity, and how it could improve their health. We would also discuss any potential risks and steps taken to mitigate them, aiming to build trust and assuage their fears.
Question 13: What do you do if a minor patient confides in you about being sexually active and requests you not to disclose this to their parents?
Expert Response: Confidentiality is crucial in the doctor-patient relationship, but so is the safety and welfare of a minor patient. In the situation presented, I would first ensure that the minor is not a victim of exploitation or abuse. I would provide them with guidance about safe sex and the potential health consequences of sexual activity. If the minor appears unable to make safe, informed decisions, or if I suspect abuse, local laws might require me to breach confidentiality and report the situation to child protective services. The ultimate goal is to protect the minor’s health and well-being.
Question 14: A relative asks you to prescribe them medication for a condition they believe they have, but you have doubts about their self-diagnosis. How do you handle this?
Expert Response: In this situation, professional boundaries are crucial. I would suggest that my relative book a proper medical consultation, during which we can discuss their symptoms and conduct necessary investigations. Only after a thorough evaluation would I prescribe medication if necessary. This ensures the right treatment is provided, and it also maintains the professional nature of our relationship.
Question 15: A patient refuses to take a medication that you believe is crucial for their recovery. How would you handle this?
Expert Response: I would engage in a candid discussion with the patient about the importance of the medication and the potential risks of not taking it. I would also listen to their concerns or fears, as there might be underlying issues like fear of side effects or cost concerns that need to be addressed.
Question 16: You find out that a colleague has made a significant error in treating a patient, and they are oblivious to their mistake. How would you handle this?
Expert Response: Ensuring patient safety is paramount. I would bring the mistake to my colleague’s attention privately and suggest ways to rectify the situation. If they refuse to acknowledge or correct their error, it may be necessary to escalate the issue to a supervisor to prevent harm to the patient.
Question 17: How would you manage a situation where a patient's cultural beliefs conflict with their medical needs?
Expert Response: Cultural sensitivity is important in medical practice. I would have a respectful discussion with the patient, aiming to understand their perspective while explaining the medical necessity of the proposed treatment. I would work with the patient to find a solution that respects their cultural beliefs but does not compromise their healthcare.
Question 18: A pharmaceutical representative offers you an all-expenses-paid trip to a conference in exchange for prescribing their company's drug. What is your response?
Expert Response: Accepting such an offer could introduce bias into my prescribing practices and undermine patient trust. I would decline the offer and maintain my commitment to prescribing based on the best available evidence and the specific needs of my patients.
Question 19: You are an oncologist, and your patient is seeking alternative treatments instead of chemotherapy due to fear of side effects. How would you handle this?
Expert Response: Addressing patient fears is crucial. I would have an open discussion about the benefits and risks of chemotherapy, and why I believe it’s the best option. I would also discuss the alternative treatments they’re considering and provide factual information about their effectiveness or lack thereof. This conversation aims to ensure the patient can make an informed decision about their care.
Question 20: As a surgeon, a patient requests that you not disclose their diagnosis to their family. How do you manage this request?
Expert Response: Patient confidentiality is a fundamental aspect of medical practice. I would respect the patient’s request while also discussing the benefits of having a support system during treatment. However, the final decision would be respected unless there are legal reasons that would mandate disclosure.
Critical Thinking MMI Questions
These questions test your problem-solving abilities and analytical skills. They may present a problem or situation and ask you to analyze the issue, formulate a solution, or discuss the implications.
Question 21: As a member of a medical team that has developed a vaccine for a new deadly disease, you discover you can only produce enough doses for 70% of the population. How do you determine who receives the vaccine?
Expert Response: A fair strategy that maximizes benefits is essential. I’d suggest prioritizing the vaccine for frontline healthcare workers, essential workers, and vulnerable populations like the elderly and those with pre-existing conditions. The subsequent distribution could be based on factors such as exposure risk. Involving stakeholders and ethics experts in the decision-making process is critical, as is transparent communication with the public.
Question 22: A 14-year-old boy refuses a life-saving surgery due to fear. How would you manage this?
Expert Response: In this case, I would invest time in understanding the boy’s fears and concerns, explaining the surgery’s importance in a way he can understand. If he still refuses, involving a child psychologist becomes necessary. We might also need to consider legal pathways to enforce the procedure if it is indeed crucial for his survival.
Question 23: A patient is refusing to take their prescribed medication due to negative online reviews. How do you approach this?
Expert Response: Misinformation is a common issue in the digital age. First, I would validate the patient’s concerns. Then, I would provide evidence-based information about the medication, its purpose, and its potential risks and benefits. It’s also crucial to address the source of their information and encourage patients to discuss any health-related information they find online.
Question 24: In a resource-limited healthcare facility, you are forced to decide between saving a 20-year-old or an 80-year-old. What factors influence your decision?
Expert Response: Such a distressing situation raises challenging ethical issues. However, when resources are scarce, one might consider maximizing life-years saved, which suggests treating the younger patient. This complex issue ideally involves an ethics committee, and we should always strive to find additional resources to avoid such choices.
Question 25: A 25-year-old terminal cancer patient is contemplating alternative treatments, but you believe that palliative care is the best approach. How do you respond?
Expert Response: While my role as a physician is to provide evidence-based advice, patient autonomy is also key. I would engage in an open discussion about her disease, the pros and cons of alternative treatments versus palliative care, and the importance of considering quality of life.
26
As a primary care physician, a patient demands antibiotics for a viral condition. How do you handle this?
27
While working in the ER, two patients arrive simultaneously, both needing immediate attention, but you can only attend to one. How do you choose?
28
A terminally ill patient asks about their prognosis, but their family has previously requested you not to disclose the disease's full extent. How do you navigate this?
29
On a medical mission in a developing country with limited medication supplies, how do you decide which patients receive the medication?
30
A patient refuses to participate in a clinical trial that could potentially benefit them. How do you respond?
31
A patient's family insists on aggressive treatment continuation for a patient who is not responding and suffering. How do you manage this situation?
32
While working in a rural area with limited resources, how do you decide on the services to provide and the patients to treat?
33
A colleague frequently takes undue credit for collaborative work. How do you address this?
34
A smoking patient has been diagnosed with lung cancer but refuses to quit. How do you respond?
35
A patient with severe pain persistently requests higher doses of opioid medication. What's your strategy?
36
A patient with a psychiatric illness refuses treatment, claiming it impairs their artistic abilities. How do you approach this situation?
37
As part of a public health campaign team, you face disagreements about the campaign's direction. How do you resolve this?
38
A patient chooses a procedure you believe is against their best interest. How do you handle this?
39
A family member wishes to donate a kidney to their relative, but they are a poor match, and the procedure carries significant risks. How do you navigate this?
40
A terminally ill patient wants to try an experimental procedure unavailable in your country. How would you manage this?
Communication Practice MMI Questions
This category evaluates your interpersonal and communication skills. Questions may revolve around explaining complex concepts in simple terms, discussing difficult topics with patients or family members, or handling conflicts or misunderstandings.
Question 41: A patient struggles with adherence to their treatment plan due to misunderstanding its importance. Your communication approach?
Expert Response: My first step is empathy, validating the patient’s concerns. Next, I simplify the treatment plan and highlight the benefits of adherence and risks of non-compliance. Encouraging questions and patient involvement in decisions improves compliance.
Question 42: You must clarify a complex medical procedure to a patient with limited health literacy. Your approach?
Expert Response: Clarity and simplicity are vital in my communication. I avoid medical jargon and use everyday analogies. I make sure the patient is comfortable to ask questions and continually verify their understanding.
43
A patient expresses anger due to a prolonged wait for their appointment. How do you handle it?
44
A colleague provides feedback that you initially disagree with. Your response?
45
You must deliver unfavorable news to a patient. Your strategy?
46
A patient's family member influences the patient's care decisions excessively. Your intervention?
47
You need to win the trust of a distressed and upset child. Your communication strategy?
48
A patient remains non-communicative and withdrawn. Your engagement strategy?
49
Despite your efforts, a patient expresses dissatisfaction with your care. Your response?
50
A colleague's habitual lateness disrupts workflow. Your communication approach?
51
A patient denies your observations of potential mental health issues. Your approach?
52
You spot a minor error in a colleague's email. Your response?
53
Language barriers hinder a patient's understanding. Your methods to ensure effective communication?
54
A colleague provides incorrect information to a patient. Your intervention?
55
An anxious family member of a patient continually interrupts your communication with the patient. Your handling strategy?
56
A patient expresses dissatisfaction with their previous doctor. Your response?
57
A patient complains about a colleague. Your management strategy?
58
A patient rejects their diagnosis, seeking a second opinion. Your response?
59
You need to persuade a patient to adopt significant lifestyle changes for their health. Your strategy?
60
Colleagues discuss a patient with inaccuracies in their conversation. Your action plan?
Teamwork and Collaboration Practice MMI Questions
These questions assess your ability to work effectively in a team. They may present scenarios involving team projects or collaborative tasks, and assess your contribution, conflict resolution skills, and your ability to collaborate with others to achieve common goals.
Question 61: Your team hits a roadblock due to disagreement on the best course of action. How do you help reach a resolution?
Expert Response: Facilitating respectful, open communication is crucial. I’d encourage everyone to share their perspectives, then evaluate each based on evidence, seeking consensus. If unresolved, we might seek external input.
Question 62: A team member consistently underperforms, affecting overall productivity. Your approach?
Expert Response: I’d have a private, constructive conversation with them, outlining the team’s concerns, inquiring about challenges they face, and exploring solutions. Fostering a supportive environment is key to peak performance.
Question 63: Some team members undervalue others' input. How do you address this?
Expert Response: I’d reinforce the importance of respect and openness, reminding the team that everyone’s unique skills and perspectives are valuable and contribute to our collective success.
Question 64: A colleague isn't contributing equally to a group project. How do you handle this?
Expert Response: Addressing the issue directly yet tactfully with the colleague is essential. I’d discuss the importance of everyone’s contribution to the project’s success. If the behavior persists, escalating it to a supervisor might be necessary.
Question 65: You disagree with your team's task approach, but they reject your alternative. How do you handle this?
Expert Response: I would understand their reasoning, present my alternative with evidence, and if they still disagree, I’d respect the decision and commit to the chosen approach. Collaboration often involves compromise.
66
A team member consistently takes credit for collective work. How do you handle this?
67
Conflict between two team members impacts morale. Your approach?
68
You suspect a team member faking their results on a research project. Your action?
69
Your team consistently misses deadlines. Your strategies to ensure timely task completion?
70
A team member frequently interrupts during meetings. How do you address this?
71
A team member doesn't respect your ideas or opinions. How do you handle this?
72
A team member frequently misses meetings without notice. Your response?
73
A team member's skills aren't effectively utilized. How do you improve this?
74
Your team leader favors one member consistently. Your handling strategy?
75
You join a team with work styles differing from yours. How do you adapt?
76
A team member's persistent negativity brings the team down. How do you address this?
77
A team member dominates conversations. How do you ensure everyone's voices are heard?
78
Your team is assigned a task beyond your collective skill set. Your handling strategy?
79
The team overlooks a member's unprofessional behavior due to their performance. Your approach?
80
Your team leader doesn't clearly communicate expectations. Your handling approach?
Empathy and Compassion MMI Interview Questions
Questions in this category evaluate your capacity for empathy, compassion, and patient-centered care. They may involve scenarios where a patient or their family is facing a difficult situation, and assess how well you respond with understanding, sensitivity, and care.
Question 81: A patient is clearly distressed about a diagnosis they have just received. How would you handle this situation?
Expert Response: It’s paramount to create a safe space for the patient to express their feelings. I’d empathize with their distress, validate their feelings, and assure them their reactions are understandable. Once they’ve shared, I’d explain the next steps and reassure them of our continuous support.
Question 82: A patient is angry and accuses you of not doing enough to help them. How would you respond?
Expert Response: Keeping calm is key. I’d listen to their grievances without interruption, validate their feelings, and apologize if needed. I’d explain the rationale behind my decisions and discuss alternatives if possible.
Question 83: A patient is non-compliant with their treatment plan. How do you handle this?
Expert Response: I’d aim to understand the root cause of their non-compliance. Whether they’re worried about side effects or don’t fully grasp the treatment’s importance, empathizing with their concerns and offering clear explanations can help them understand the value of the treatment plan.
Question 84: A patient receives a terminal diagnosis and asks, "Why me?" How would you respond?
Expert Response: This question requires great sensitivity. I’d validate their emotions, show empathy, and let them know it’s okay to feel upset and confused. I’d offer to answer any questions they have about the diagnosis or what comes next.
Question 85: A patient is frightened about an upcoming surgical procedure. How would you handle this?
Expert Response: I’d validate their fear, provide detailed information about the procedure, address their worries, and reassure them that our team is dedicated to their well-being and a successful outcome.
86
A patient with limited English struggles to understand their diagnosis. How do you handle this?
87
A patient's family interferes with their care. How would you approach this situation?
88
A patient's cultural beliefs prevent them from seeking necessary medical help. Your approach?
89
A terminally ill patient doesn't want their family to know about their diagnosis. How do you handle this?
90
A patient refuses to follow a treatment plan due to its interference with their lifestyle. How do you handle this?
91
A patient grieves the loss of a loved one. How would you comfort them?
92
A patient expresses suicidal thoughts. How do you handle this situation?
93
A patient refuses to take a certain medication due to its side effects. How do you handle this?
94
A patient feels overwhelmed by their treatment plan. How would you handle this?
95
A child patient fears injections. How would you comfort them?
96
A patient constantly misses appointments. How would you deal with this?
97
A patient is upset because their treatment isn't showing expected results. How would you handle this?
98
A patient struggles with a chronic illness's psychological impact. How would you support them?
99
A patient is in denial about their health condition. How would you handle this?
100
A patient's religious beliefs prevent them from accepting a life-saving treatment. How would you handle this situation?
Cultural Competence MMI Questions
This category measures your understanding and respect for cultural diversity in healthcare. MMI Questions may involve scenarios where cultural differences impact patient care, and assess your ability to provide respectful and appropriate care to patients of diverse backgrounds.
Question 101: How would you approach a patient whose cultural beliefs conflict with the recommended course of treatment?
Expert Response: Recognizing cultural differences is key to establishing a patient-provider relationship. I would approach this by first trying to understand the patient’s perspective. I’d ask about their beliefs and try to find a treatment approach that respects their values and also ensures their health. Collaboration with colleagues, cultural liaison officers, or religious representatives may also be necessary.
Question 102: What strategies would you use to overcome language barriers with a patient?
Expert Response: Language barriers can significantly impact the quality of care. If faced with such a situation, I would use professional medical interpreters rather than relying on a patient’s family or friends, to ensure clear and unbiased communication. Visual aids, simple language, and confirmation of understanding are also useful strategies.
Question 103: You are treating a patient who follows a traditional diet that is contributing to their health problems. How do you handle this?
Expert Response: Diet is often deeply intertwined with cultural practices. I would approach this conversation with sensitivity, acknowledging the importance of their traditional diet. Then, I’d discuss how certain aspects might be impacting their health and work with the patient to find alternatives or modifications that can align with their culture and improve their health.
Question 104: How would you handle a situation where a patient's religious beliefs prevent them from seeking necessary medical treatment?
Expert Response: In this situation, understanding and respect are paramount. I would discuss their concerns and provide clear information about why the treatment is necessary. If they continue to refuse, I’d explore alternative treatments that might align with their beliefs. Involving religious leaders or the ethics committee may be helpful in such situations.
Question 105: A patient from a minority background feels uncomfortable with the predominantly white medical staff at your clinic. How would you address their concerns?
Expert Response: Feeling comfortable with healthcare providers is crucial for the patient experience. I’d empathize with their feelings, ensuring that their concerns are heard. Then, I would discuss these issues with the team to foster a more inclusive environment. Offering to connect the patient with healthcare providers from similar backgrounds, if available, might also help them feel more comfortable.
106
How would you approach a situation where a patient's cultural practices could potentially harm their health?
107
You are treating a patient who prefers traditional healing methods over modern medicine. How do you handle this?
108
How would you handle a situation where a patient's family is interfering with their care due to cultural beliefs?
109
You are treating a patient who does not believe in vaccinations due to their religious beliefs. How would you handle this?
110
How would you approach a patient who is reluctant to discuss their health due to cultural stigmas associated with illness?
111
How would you handle a situation where a patient's cultural beliefs prevent them from seeking mental health treatment?
112
You are treating a patient who refuses a blood transfusion due to their religious beliefs. How would you handle this?
113
How would you deal with a patient who insists on having a family member of the same gender present during physical examinations due to cultural reasons?
114
How would you handle a situation where a patient's cultural practices involve the use of potentially harmful substances?
115
A patient's cultural beliefs are causing them to refuse palliative care for a terminal illness. How would you handle this?
116
How would you approach a situation where a patient's religious beliefs interfere with the agreed-upon treatment plan?
117
You are treating a patient who wants to incorporate traditional healing practices into their treatment plan. How would you handle this?
118
A patient from a different cultural background is struggling to trust the medical team. How would you handle this?
119
How would you approach a situation where a patient's cultural beliefs are leading them to avoid regular health check-ups?
120
You are treating a patient whose cultural practices involve fasting, which is affecting their health. How would you handle this?
Personal Experiences
These questions are about your personal and professional experiences, aiming to understand your motivations, values, resilience, and reactions to certain situations. They may ask you to reflect on specific experiences or discuss how these experiences have shaped you.
These questions are designed to assess your personal qualities, experiences, and how they shaped your decision to pursue a career in medicine.
Question 121: Would you mind sharing an experience where you made a difficult decision and what you learned from it?
Expert Response: I recall my senior year in college when I found myself juggling my role as the student council president along with my challenging pre-med coursework. At one point, managing both was impacting my academic performance. I was faced with a difficult decision – to resign from the council or risk my grades. I chose to prioritize my studies. The experience highlighted the importance of understanding my limitations and prioritizing tasks.
Question 122: How have your experiences as a volunteer shaped your perspective on healthcare?
Expert Response: Volunteering at a local clinic in an underprivileged neighborhood brought to light the gaps in healthcare accessibility. This experience solidified my belief that healthcare is a fundamental right, and inspired me to champion equal access throughout my medical career.
Question 123: Could you talk about the challenges you've faced on your journey to medical school and how you overcame them?
Expert Response: One of the most significant challenges I faced was maintaining my academic responsibilities while dealing with a personal crisis – a family member fell ill during my undergraduate studies. I learned to manage my time effectively and build resilience. This experience underscored the importance of mental well-being, self-care, and the need for a strong support network.
Question 124: Could you share a time when you had to work as part of a team to achieve a common goal?
Expert Response: During a group research project, we faced disagreements about the research direction. I proposed that we refocus on our common goal and led a discussion to understand each team member’s perspective. Ultimately, we agreed on a path that represented our collective interests.
Question 125: Could you describe a time when you received constructive criticism, how you responded, and what you learned?
Expert Response: In one of my biology classes, my professor noted that my analysis often lacked depth. Although my initial reaction was defensive, I soon realized that this feedback was an opportunity to grow. I worked on improving my analytical skills, and by the end of the semester, I had significantly improved my grade. This experience taught me the importance of being open to and learning from constructive feedback.
Question 126: Can you tell me about a time when you had to step up and lead?
Expert Response: Absolutely! When I was in college, I led a team for a group assignment. I had to keep everything organized, set deadlines, and make sure everyone was on the same page. It really helped me sharpen my leadership and organizational skills. Plus, it taught me the importance of trust when delegating tasks to team members.
Question 127: Ever stumbled and fell? What did you learn from a major failure?
Expert Response: Yes, definitely. In my first year at college, I bombed an important organic chemistry exam. But I didn’t let it get me down. Instead, I got some tutoring and put in more hours studying. The extra effort paid off, and my grade improved a lot in the next exam. It was a good lesson in how failure can motivate us to improve.
Question 128: Can you share a story about adapting to a different environment or culture?
Expert Response: Sure! I spent a gap year volunteering at a clinic in a rural part of a developing country. It was a total culture shift and the clinic was lacking resources. I had to adapt and learn to respect different cultural viewpoints. Also, I had to think on my feet to tackle healthcare challenges in that setting.
Question 129: How did your past experiences shape your decision to go into medicine?
Expert Response: Well, my parent is a nurse, so I had an early introduction to healthcare. Seeing their dedication to patients was really inspiring. Then, when I volunteered at a local clinic, I realized that I wanted to help people through medicine too. These experiences made me see the difference that healthcare professionals can make, and that motivated me to pursue a career in medicine.
Question 130: Could you tell about a time when you went above and beyond to help someone out?
Expert Response: Sure thing! When I was volunteering at a senior care home, I met a resident who was pretty lonely and didn’t join in activities. I decided to spend extra time with her, just listening to her stories and playing her favorite games. Eventually, she started to join in more with the group activities. This taught me that small acts of kindness can make a big difference in someone’s life.
131
Share an experience where you had to handle a high-pressure situation.
132
How have your experiences with diversity shaped your perspective?
133
Can you describe an instance where you had to resolve a conflict?
134
Describe an experience where you had to step out of your comfort zone.
135
Share an example of how you demonstrated resilience in the face of adversity.
136
Can you describe an experience where you made a positive impact on someone's life?
137
How have your academic experiences prepared you for medical school?
138
Describe a situation where you demonstrated empathy.
139
Can you share an experience where you demonstrated excellent communication skills?
140
Share an experience that tested your ethics and how you handled it.
Healthcare and Policy Knowledge
This section looks into your grasp of the healthcare system and policies. It could revolve around ongoing healthcare subjects, policy issues, or trends, aiming to gauge your ability to engage in informed and considerate discussion.
Question 141: How could we make healthcare more accessible to disadvantaged communities?
Expert Response: Improving healthcare accessibility isn’t a one-step solution. It could involve bolstering community health centers in underprivileged areas. Telemedicine also has huge potential for delivering healthcare remotely. Additionally, we should concentrate policy efforts on expanding insurance coverage and making it more affordable.
Question 142: How do you see the current state of mental health care?
Expert Response: We’ve seen improvements in mental health care in recent years, but there’s a lot of work ahead. Issues around access, stigma, and funding persist. It’s crucial that we prioritize mental health services, weave them into primary care, and enhance public awareness to tackle stigma.
Question 143: What strategies could help to curb the escalating healthcare costs?
Expert Response: To mitigate escalating healthcare costs, an emphasis on preventive care is vital; it helps control chronic diseases. We also need to push for price transparency, which can stimulate competition and bring prices down. Additionally, enhancing healthcare efficiency through minimizing administrative costs and waste can contribute significantly.
Question 144: How do you feel about technology's role in healthcare?
Expert Response: Healthcare technologies like electronic health records and telemedicine hold great promise for enhancing patient care. However, these also bring forth concerns about data security and equal access. As future healthcare professionals, we should welcome technological advancements while being conscious of these issues.
Question 145: What steps should we take to tackle the opioid crisis in the U.S.?
Expert Response: Tackling the opioid crisis necessitates a multifaceted approach. This includes education on safe opioid use, improved prescribing practices, broadening access to opioid addiction treatment, and expanding the use of naloxone to reverse opioid overdoses.
Question 146: How could we reshape the U.S. healthcare system to enhance accessibility?
Expert Response: Enhancing accessibility in the U.S. healthcare system is a complex issue requiring a diverse approach. Possible strategies include investing in preventative care, backing the expansion of telemedicine, advocating for policy changes for more affordable healthcare, and addressing social determinants of health causing accessibility barriers.
Question 147: What's your view on legalizing euthanasia or physician-assisted suicide?
Expert Response: This is a deeply sensitive issue with compelling arguments on both ends. Personal autonomy and relief from suffering stand for euthanasia. However, there are potential ethical and legal implications, like life sanctity and possible misuse or coercion. Hence, comprehensive and transparent dialogues on these issues are crucial to guide policy decisions.
Question 148: What could be the outcomes of introducing a single-payer healthcare system in the U.S.?
Expert Response: Introducing a single-payer healthcare system could lead to various outcomes. It might enhance accessibility and simplify administrative procedures. However, financial feasibility concerns, potential for extended wait times, and the impact on care quality need to be addressed. It’s a multifaceted issue demanding careful thought.
Question 149: Where do you stand on compulsory vaccinations?
Expert Response: Compulsory vaccinations are a vital public health measure to prevent infectious disease spread. However, individual autonomy and religious or personal beliefs need due respect. Balancing public health with personal freedoms is a challenge, and I believe policies of this nature should always be accompanied by education and awareness.
Question 150: In your view, how has COVID-19 influenced healthcare's future?
Expert Response: The COVID-19 pandemic has undeniably left a significant mark on healthcare. It has expedited the use of telemedicine, underlined the value of public health and preventative care, and revealed our healthcare systems’ vulnerabilities. These lessons can guide changes to make our healthcare systems more robust in the future.
151
What should our approach be to deal with physician burnout?
152
How does health policy impact patient care?
153
How important is preserving patient privacy and confidentiality?
154
What's your take on universal healthcare?
155
How should healthcare professionals handle the anti-vaccination movement?
156
How does cultural competence influence healthcare delivery?
157
What might be the implications of genetic testing?
158
How can the healthcare system better cater to the needs of an aging population?
159
How does socioeconomic status affect health outcomes?
160
What impact does climate change have on health?
Role Play
In these stations, you may be asked to assume a particular role in a simulated situation. This could involve interacting with an actor who plays a patient, family member, or colleague. The goal is to assess your communication skills, empathy, professionalism, and adaptability.
Question 161: Role-play a situation where you have to break bad news to a patient.
Expert Response: When breaking bad news, it’s crucial to be empathetic, honest, and supportive. I would ensure a private and comfortable environment, then deliver the news in a clear, concise manner, allowing the patient to process the information. I’d also offer emotional support and discuss the next steps.
Question 162: You are a doctor, and a child's parents refuse to vaccinate their child due to misinformation. How do you handle this?
Expert Response: It’s important to approach this conversation with empathy and understanding. I would calmly address their concerns, provide accurate information about the safety and benefits of vaccines, and stress the potential risks of not vaccinating. Ultimately, I must respect their decision while advocating for the child’s health.
Question 163: Role-play a situation where you have to communicate a treatment plan to a patient with a language barrier.
Expert Response: Communication is key in healthcare. In this situation, I would enlist the help of a professional medical interpreter or use visual aids to ensure the patient understands their treatment plan. I’d also encourage them to ask questions to verify their understanding.
Question 164: A patient under your care has misunderstood their diagnosis and is unnecessarily worried. How do you address this?
Expert Response: I would approach this with sensitivity and patience. It’s important to reassure the patient and correct the misunderstanding. I’d explain the diagnosis in simple, clear language, focusing on the facts while also addressing their concerns.
Question 165: Role-play a situation where a colleague makes a racist comment. How do you handle it?
Expert Response: Addressing such behavior is crucial for promoting a respectful and inclusive environment. I would calmly express my disapproval of the comment, explaining why it’s inappropriate. Afterwards, I’d report the incident to a superior or HR, as racism should not be tolerated in the workplace.
166
Role-play a situation where a patient is angry and yelling at the staff.
167
You are a doctor, and your patient does not want to follow your recommended treatment plan. How do you handle this?
168
Role-play a situation where you have to work with a difficult team member.
169
A patient's family member asks you to withhold the patient's diagnosis from them. How do you handle this?
170
Role-play a situation where a patient is non-compliant with their medication regimen.
171
You are a medical student, and you've made a mistake during your clinical rotation. How do you handle this?
172
Role-play a situation where you need to address unprofessional behavior in a peer.
173
A patient questions your competence due to your young age. How do you respond?
174
Role-play a situation where you need to address a gap in communication between members of a healthcare team.
175
You have to inform a patient that their treatment is not working as expected. How do you deliver this news?
176
Role-play a situation where you have to mediate a conflict between two colleagues.
177
A patient asks for your personal opinion about a controversial medical treatment. How do you respond?
178
Role-play a situation where a patient's family has unrealistic expectations about the patient's prognosis.
179
You are a doctor, and you disagree with a colleague's treatment plan for a mutual patient. How do you handle this?
180
Role-play a situation where a patient repeatedly misses their appointments.
Scenario-Based Questions
These questions present a situation or task that you have to deal with, such as managing a medical emergency, handling a conflict, or dealing with a stressful situation. They test a range of competencies, including problem-solving, stress management, ethical judgment, and communication.
These questions present you with a hypothetical situation and ask you to analyze it or determine a course of action.
Question 181: Consider a situation where a patient with a DNR order goes into cardiac arrest and a new nurse, unaware of the order, starts CPR. How would you respond to this situation?
Thoughtful Answer: This is a sensitive scenario. The patient’s wishes must be respected, so I’d immediately inform the nurse of the DNR order. To avoid such future instances, I’d promote enhanced communication protocols about DNR orders within the team.
Question 182: Imagine stumbling upon a social media post where a friend of yours discusses self-harm. What steps would you take?
Insightful Answer: Firstly, I’d reach out to my friend directly to express my worry and suggest professional assistance. If they were unresponsive or I perceived immediate danger, I’d contact appropriate emergency services or a mental health crisis line.
Question 183: You're in a group project, and one member isn't pulling their weight. How would you deal with this?
Analytical Answer: I’d privately converse with the individual about their lack of contribution, trying to understand any underlying problems. If this doesn’t bring change, I’d bring up the issue with the team, advocating for a solution that maintains fairness and collaboration.
Question 184: Your boss assigns you a task that exceeds your skill level. How do you react?
Practical Answer: Open communication is key here. I’d express my concerns to my supervisor, suggesting possible alternatives like obtaining further training or assigning the task to a colleague with the necessary skills.
Question 185: If you witnessed a car accident involving a close friend who was at fault, and later you're called as a witness, how would you act?
Honest Answer: While it would be difficult, I would recount the incident objectively and truthfully. It’s crucial to honor the legal process and recognize the consequences of my friend’s actions.
186
A terminally ill patient, who is in pain and has voiced a desire to pass away, is being subjected to aggressive treatment because of the family's insistence. How would you react?
187
You spot a fellow student cheating during an examination. What's your course of action?
188
A patient with a significant allergy to peanuts has accidentally consumed some peanuts. What is the immediate step you would take?
189
A pharmaceutical corporation offers you a fully-funded trip to a conference on the condition that you prescribe their latest medication. What is your response?
190
Your team is on a project, and a member consistently monopolizes the conversation, not allowing others to share their ideas. How would you handle this situation?
191
A patient suffering from advanced Alzheimer's disease consistently refuses to eat. What strategy would you use to manage this situation?
192
A parent declines potentially life-saving treatment for their child because of their personal beliefs. What is your response to this?
193
You observe a colleague showing up to work under the influence. What actions would you take in this situation?
194
A patient is requesting a treatment option that you believe isn't in their best interest. How do you handle this circumstance?
195
A senior doctor commits a mistake that could potentially harm a patient but doesn't acknowledge it. What actions do you take?
196
A colleague casually shares confidential patient information with you. What is your response?
197
The family of a patient, who is not currently conscious, is pushing for aggressive treatment that the patient has previously refused. What do you do?
198
You've made an error that hasn't yet affected patient care, but there's a potential it could in the future. How do you handle this?
199
A patient's family invites you to join them in prayer, but you do not share their religious beliefs. How would you handle this situation?
200
A coworker makes an inappropriate sexist remark. How do you respond to this?
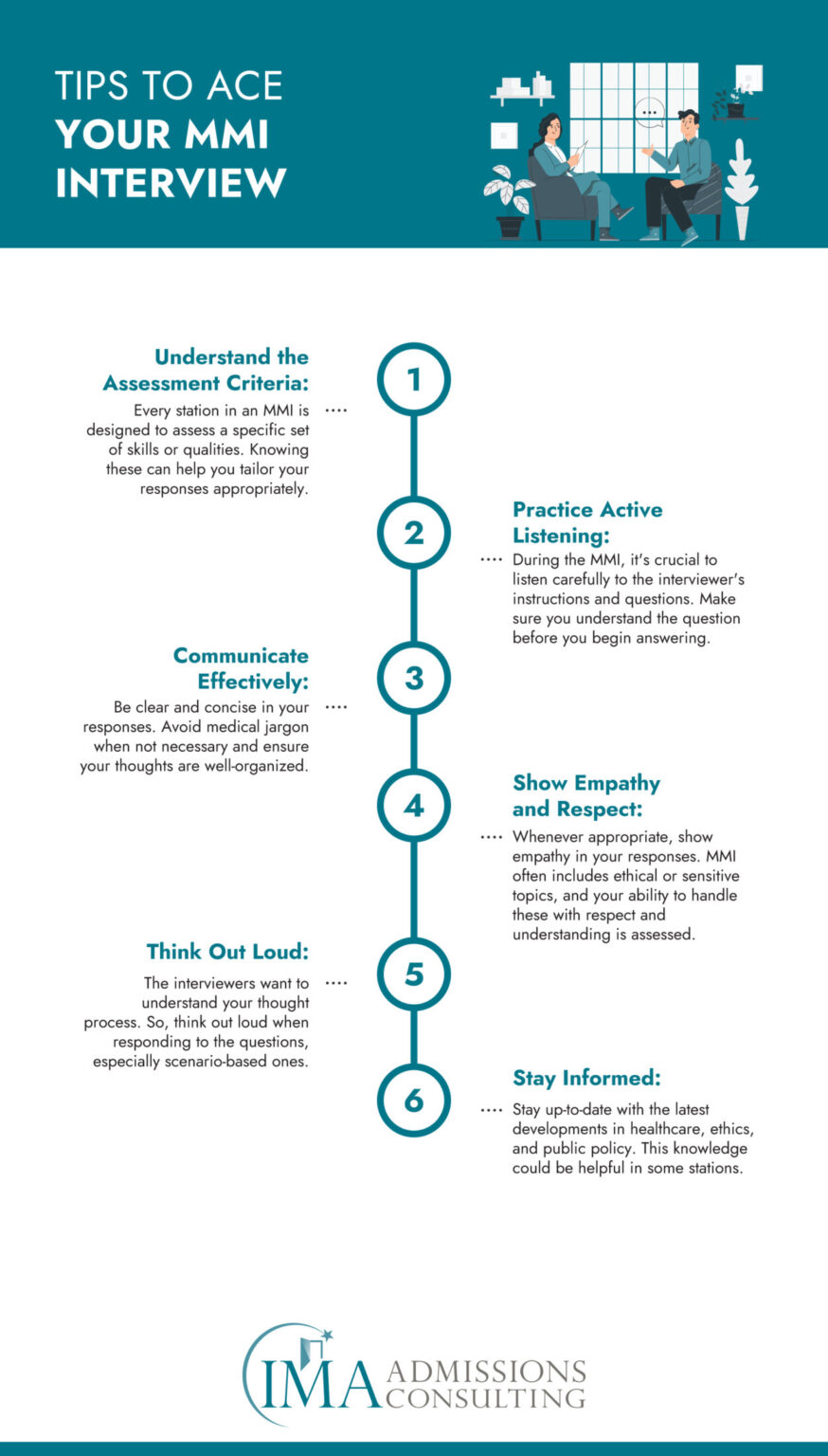
Tips to Ace Your MMI Interview
Just like any other interview, the key to acing an MMI interview lies in meticulous preparation and strategic execution. Here are some tips to help you excel in your MMI:
A pre-med shadowing study abroad program can provide invaluable experience and knowledge, which can greatly aid in the MMI interview. In these programs, you have the opportunity to observe healthcare delivery in a different cultural and socio-economic context, thereby broadening your perspective. This experience can help you answer questions more insightfully and also showcase your commitment to understanding global healthcare.
MMI Interview Questions FAQs
In this section, we will address some frequently asked questions about the MMI interview process.
What is the purpose of MMI interview questions?
The MMI is designed to evaluate skills like communication, empathy, and ethical decision-making, which are not necessarily reflected in grades and test scores.
What should I wear to an MMI interview?
Dress professionally as you would for a job interview. This usually means a suit and tie for men, and a suit, dress, or skirt and blouse for women.
How should I prepare for MMI interview questions?
Understanding the format and question types of MMI, reflecting on your experiences, and practicing MMI questions are all crucial in your preparation. Medical school admissions consulting can also greatly aid in your preparation.
Can I make a mistake in an MMI?
Yes, MMI is designed to be challenging and it’s normal to have stations where you feel you didn’t perform your best. However, remember that each station is scored separately and one mistake does not affect your performance on the other stations.
What happens if I finish my response before the time is up?
It’s okay to finish early if you’ve answered the question effectively. Don’t ramble on just to fill the time. Use the extra time to summarize your main points or to ask the interviewer if they have any questions.
Remember that every MMI interview might be slightly different based on the medical school conducting it. Do your research about the specific school and reach out to school admissions consulting for personalized guidance.
The Role of Medical School Admissions Consulting in MMI Interviews
Medical school admissions consulting plays a crucial role in preparing for MMI interviews. Expert consultants are often well-versed with the format and know what medical schools are looking for in applicants. They can provide valuable guidance, tips, and feedback to improve your responses. They can also provide practice MMI questions, simulating real interview conditions, and helping you get comfortable with the process.
Medical schools near me and you often provide detailed information about their interview process on their websites. So, research these schools and use them to fine-tune your preparation process with the help of admissions consulting.
It’s crucial to remember that MMI interviews are not just about right answers but about showcasing the qualities that make you a good fit for a career in medicine. Medical school admissions consulting can help you highlight these qualities effectively.
How to Seek Help
Preparing for MMI interview questions can seem daunting, but you don’t have to do it alone. International Medical Aid (IMA) offers a comprehensive range of services, including a pre-med shadowing study abroad program, school admissions consulting, that can significantly improve your MMI interview questions performance. Our team of experienced consultants can provide valuable insights, tailored advice, and rigorous practice sessions to ensure you’re fully prepared for your MMI interview questions.
If you’re ready to ace your MMI interview, schedule an appointment with IMA today. We are here to support you through every step of your medical school admissions journey.
Conclusion
MMI interview questions are a crucial part of the medical school admissions process, but with the right preparation and approach, it’s a hurdle that can be successfully navigated. From understanding the MMI format to practicing MMI questions, and seeking the guidance of medical school admissions consulting, every step you take in preparation is a step closer to your career in medicine.
Remember, the MMI is not just about answering questions but showcasing your skills, values, and character. As you prepare, reflect on your experiences, stay informed about healthcare issues, and above all, remain authentic in your responses. And remember, IMA is here to help you with your MMI preparation. You’re not alone in your journey, so reach out and let’s conquer the path to medical school together!