The World Health Organization, for the second time since 2022, has declared a worldwide emergency. In just two months, monkeypox spread to over 65 countries, with the average number of confirmed cases per day jumping from below one in May to over 600 by the end of July. This 2022 monkeypox outbreak is the first time the disease has spread extensively outside of West and Central Africa.
What is Monkeypox?
Monkeypox — which shares an evolutionary lineage with smallpox, a far more deadly poxvirus — is spread through contact with infected skin, bodily fluids, or infected animals. Monkeypox is also transmissible through airborne respiratory droplets, though airborne transmission is rare and relatively under-researched as of July 2022. The current outbreak of monkeypox in European and North American countries is primarily spreading amongst men who have sex with men.
Monkeypox was first reported in humans in the Democratic Republic of Congo in 1970, though the disease was first observed in laboratory monkeys in Denmark in 1953. Until recently, the virus has mostly been endemic to ten Central and Western African countries. Other monkeypox outbreaks include a 2003 outbreak in the U.S. traced to imported rodents, and a 2017 outbreak in Nigera — which occurred after the country had reported zero cases for over 30 years.
The smallpox vaccine can be used to prevent monkeypox infection. Some health experts contribute the decades of monkeypox presence in Africa to the continent’s lack of access to global stockpiles of smallpox vaccines.
The monkeypox strain active in the 2022 monkeypox outbreak has a fatality rate of around 1% but has risen as high as 3%. Most people infected with monkeypox experience rashes, fevers, and swollen lymph nodes and recover in a few weeks.
Monkeypox is Getting a New Name
In June 2022, the WHO Director General announced that monkeypox would be renamed. The decision comes in response to a group of international scientists calling attention to its discriminatory and stigmatizing name. Current WHO guidelines discourage naming diseases after regions or animals. The WHO advises that naming diseases should be done in a way that minimizes offending any regional, cultural, professional, ethnic, national, or religious groups.
The name “monkeypox” was given to the disease after being discovered among laboratory monkeys in 1958 in Copenhagen, Denmark. It wasn’t until 1970 that the disease was observed in humans. Although monkeypox was first found in monkeys, the original animal source of the disease is unknown — monkeys, like humans, are simply carriers of the disease. Many researchers speculate that rodents play a significant role in the transmission of monkeypox to humans
Transmission
Monkeypox is a contagious disease and there are several modes of transmission. Generally, monkeypox is spread from person to person through:
- Contact with infected lesions
- Contact with infected bodily fluids like saliva, semen, or blood
- Breathing in infected respiratory droplets
Monkeypox can also be spread among humans through objects that have come into contact with infected rashes or bodily fluids. This kind of transmission is less likely.
2022 Monkeypox Outbreak Transmission Trends
Research published in the New England Journal of Medicine reports that 98% of people diagnosed with monkeypox between April 27 and June 24, 2022, were bisexual or gay men. The research suggests that 95% of monkeypox cases in this timeframe were contracted through sexual activity.
Pets and Animals
Animal-to-human transmission has historically occurred through bites or scratches. Eating or preparing food with the meat or byproducts of an infected animal can also transmit the disease.
While research into other forms of animal-to-human and human-to-animal transmission is still ongoing, the CDC cautions that monkeybox could be spread between people and animals through:
- Sharing food or sleeping areas
- Licking and kissing
- Cuddling and petting
It’s still unclear to researchers whether or not monkeypox can be spread from humans to dogs or cats. As a precaution, pet owners should assume it can be spread to any mammal. If you have monkeypox symptoms, avoid contact with your pets and wildlife until you’re cleared by a doctor.
If your pet has not been exposed to monkeypox but someone in your household is showing symptoms, ask friends or family members to take care of the pet in a different environment until the disease has run its course. Disinfect your home before bringing the pet back.
Keep pets that have been exposed away from people and other animals for 21 days and avoid close contact. Don’t care for a pet if you are infected with monkeypox, even if the pet has already been exposed.
If anyone in your home is at increased risk for severe symptoms, you should avoid caring for an infected pet. This includes:
- People who have or have had eczema or dermatitis
- People who live with children 8 years old or younger
- People who are pregnant
- People who are immunocompromised
If you must care for pets while you’re infected with monkeypox, make sure to cover rashes and lesions and wear gloves and a mask while handling the animal. Wash your hands thoroughly before and after contact. Keep your pet from clothes, bedding, and any other objects that may have been in contact with infected rashes, bodily fluids, or open wounds.
Signs and Symptoms
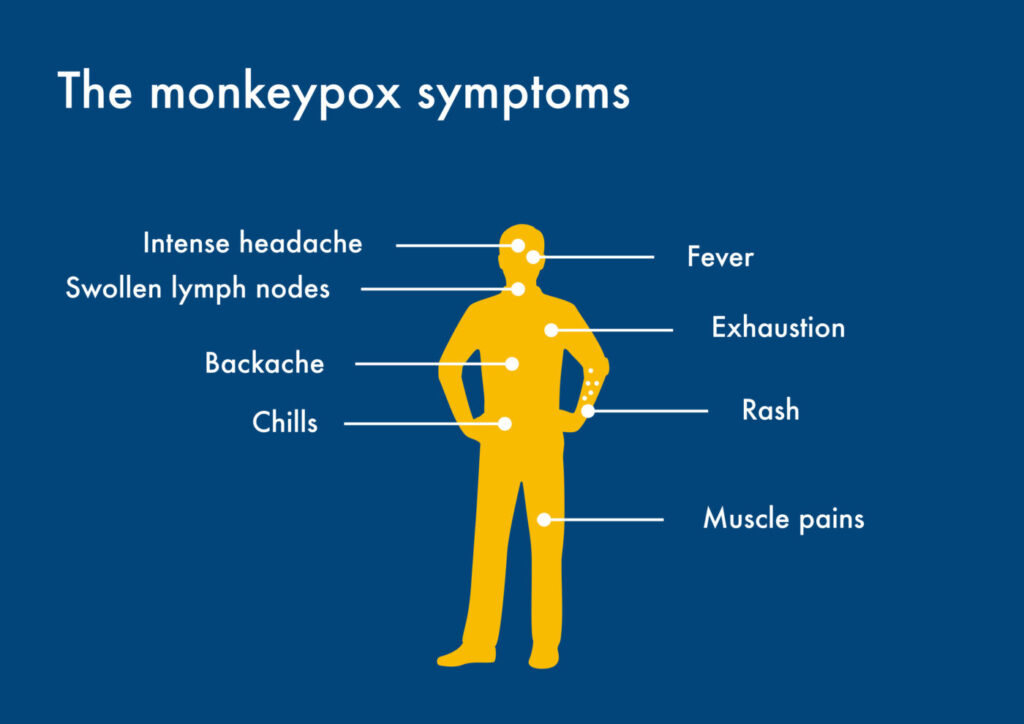
Monkeypox symptoms usually appear within 6-13 days. The incubation period can range from 5-21 days. Generally, the symptoms of monkeypox are similar to, yet milder than, chickenpox.
Early symptoms may consist of fatigue, muscle aches, swollen lymph nodes, fever, back pain, sore throat, dry cough, and intense headaches. The presence of lymphadenopathy (swollen lymph nodes) makes monkeypox distinct from other poxes, such as chickenpox.
Within 1-3 days of getting a fever, rashes and eruptions begin to appear. In most instances, rashes are concentrated on the face and limbs. In 95% of reported monkeypox cases, rashes appear in the face, in 75% they appear on the palms of the hands or the soles of the feet, and in 70% rashes appear in the mucous membranes in the mouth. In 30% of cases, rashes appear on genitalia. The eyes are affected in 20% of cases, specifically the conjunctivae and the cornea.
In some cases, rashes appear before the other symptoms. In others, a rash appears with no symptoms.
Monkeypox rashes evolve over the course of the inflection. Red macules appear in the beginning stage. Macules are flat rashes and don’t have raised bumps. The macules turn into firm, raised legions (papules), lesions with clear fluid (vesicles), and then lesions with yellow fluid (pustules). Eventually, the lesions dry up and fall off.
Infections produce a range of a few to thousands of lesions on the infected person. If the case is severe enough, the lesions form large sections of dead tissue which slough off.
The severity of the infection depends on the amount of exposure and underlying health problems. Children are more likely to develop severe symptoms. Loss of vision due to an infected cornea, encephalitis, sepsis, and bronchopneumonia are some of the more serious complications that can arise.
Scientists are currently unsure of the number of asymptomatic infections.
New Symptoms
Doctors have identified a few new symptoms associated with the current outbreak, some of which are mentioned above. These newly identified symptoms are not traditionally part of what defines monkeypox. New symptoms include:
- Rash appears before fever or fever never develops
- Bumps may be in different stages, even in the same area
- Open sores, pus-filled lesions, and bumps that resemble blisters
- In some cases, only 1-3 bumps appear
- Rashes first appear around the anus, genitals, and pubic area
Some new cases have also included tenesmus, proctitis, and bleeding in the lower intestine.
What’s causing the shift in symptoms? Scientists are unsure but research is underway.
Treatment and Prevention
Monkeypox is a self-limiting disease, meaning that it will eventually go away on its own. There is no specific cure or treatment. Treatment focuses on relieving symptoms and preventing secondary infections.
Patients are typically isolated to prevent the spread of the disease. In severe cases, patients may be hospitalized for supportive care, which may include fluids, pain relief, and oxygen therapy.
Smallpox vaccines and antivirals are also effective against monkeypox. The antiviral TPOXX is used with people at risk of exposure and at risk of developing severe symptoms, such as immunocompromised individuals.
The smallpox vaccine is recommended by the CDC for people who have been exposed to monkeypox and people who are at greater risk of developing severe symptoms. This includes
- Anyone who has been labeled as a contact of someone with monkeypox by public health officials
- Those with sexual partners who have been diagnosed with monkeypox
- Those who have had multiple sexual partners in an area where monkeypox is present
- People who work in environments that could expose them to poxvirus diseases, such as some lab workers and healthcare workers
Monkeypox can be prevented by avoiding contact with infected animals and people, which includes avoiding contact with bedding or clothing that has been used by an infected person.
In Central and West Africa, primates and rodents are common monkeypox carriers. Avoiding contact with these animals can help prevent the disease, including dead or sick animals and their bedding. The CDC keeps a list of animals that can spread monkeypox to avoid in these regions.
If you have a rash or other symptoms associated with monkeypox, you should isolate yourself from other people and contact your doctor or healthcare provider for a diagnosis..
Outlook and Containment Efforts
As of the end of July 2022, the U.S. nears 3,000 cases of monkeypox. The federal government is considering declaring a national emergency in line with the World Health Organization’s recent announcement that the rapid spread of monkeypox has become a “Public Health Emergency of International Concern.”
The CDC is working with health departments and partners to contain the outbreak and prevent further spread. Isolation, contact tracing, and vaccination are key containment strategies. The smallpox vaccine is effective against monkeypox, and the CDC recommends that people who have been exposed to the virus be vaccinated.
Containing monkeypox is challenging because of the long incubation time. Since people may be infected for up to 21 days before developing symptoms, they can unknowingly spread the disease during this time. This is why many public health experts are calling for advanced contact tracing measures. Contact tracing would allow health officials to promptly notify people who may have been exposed to the virus and help them take steps to prevent spreading the disease and seek testing and treatment.
Some public health experts and journalists are concerned about an insufficient amount of monkeypox tests leading to underreporting. Limited testing combined with rapidly rising case counts can often suggest that an outbreak is larger than the numbers indicate.
Many confirmed cases also report that patients diagnosed with monkeypox often don’t know from who they caught the infection. Additionally, many confirmed cases involve patients who believe they haven’t come into contact with people with monkeypox. This could suggest that transmission is occurring through asymptomatic carriers. In any event, being unable to trace the source of infectious diseases can make containment more difficult.
As western countries organize to combat the spread of monkeypox, many are looking to African doctors and researchers for guidance. African scientists have been monitoring and researching the disease for decades, and their expertise is crucial to understanding how to best contain the outbreak.
The U.S. is in the process of expanding testing and plans to produce another 1.6 million vaccines in the coming months.