As a medical student or prospective student, choosing a specialty is one of the most significant decisions you will make in your career. Two of the most foundational and rewarding fields in medicine are primary care and family medicine. While these terms are often used interchangeably, they represent distinct paths with unique scopes of practice. Knowing the differences and similarities between primary care and family medicine will help in guiding your decision on which type of doctor you want to become.
Primary Care Overview - What is Primary Care?
Primary care is a broad category of healthcare that focuses on the general medical needs of patients. As a primary care physician (PCP), you would be the first point of contact for patients, providing a wide range of services that include preventive care, diagnosis and treatment of common illnesses, and ongoing management of chronic conditions. Primary care physicians play a critical role in the healthcare system by coordinating patient care, making referrals to specialists when necessary, and emphasizing preventive measures to maintain patient health.
Family Medicine Physicians
Role and Scope of Practice
Family medicine physicians are specialists trained to provide comprehensive healthcare to individuals of all ages, from newborns to the elderly. Their training covers a broad range of medical areas, including pediatrics, internal medicine, obstetrics and gynecology, and geriatrics. This diverse training enables them to treat various conditions, offer preventive care, manage chronic diseases, and address acute health issues.
Patient Care Approach
Family physicians often build long-term relationships with their patients, sometimes treating multiple generations within the same family. This continuity of care allows them to develop a deep understanding of their patients’ health histories, lifestyle factors, and familial health trends. Family medicine physicians emphasize holistic care, often considering social, environmental, and psychological factors when diagnosing and treating patients.
Settings and Specializations
Family medicine physicians can work in various settings, including private practices, community health centers, and hospitals. Some may choose to further specialize in areas like sports medicine, geriatrics, or palliative care, depending on their interests. Their broad skill set also makes them valuable in rural or underserved areas where they may be the primary healthcare providers available.
Internal Medicine Physicians
Focus and Expertise
Internal medicine physicians, also known as internists, specialize in the care of adults. Their focus is on the prevention, diagnosis, and treatment of a wide array of adult illnesses, ranging from acute conditions like infections to chronic diseases such as diabetes and hypertension. Internists are often seen as problem solvers who manage complex patient cases involving multiple coexisting conditions.
Training and Specialization
The training for internal medicine physicians is extensive and includes a broad understanding of all adult organ systems. Many internists choose to subspecialize in fields like cardiology, gastroenterology, or oncology, where they focus on specific organs or disease processes. However, general internists provide comprehensive care and often serve as primary care physicians for adults, coordinating treatment across multiple specialties when necessary.
Role in Healthcare System
Internal medicine physicians typically work in hospitals, outpatient clinics, or academic settings. They are crucial in managing the health of adult populations, particularly in the context of chronic disease management, and often act as the primary point of contact for adult patients navigating the healthcare system.
Pediatricians
Specialization in Child Health
Pediatricians specialize in the medical care of children, from birth through adolescence. Their training equips them to address the unique physiological and developmental needs of children, including growth milestones, vaccinations, and early detection of congenital conditions. Pediatricians are experts in child-specific health issues, such as pediatric asthma, developmental disorders, and childhood infections.
Developmental and Preventive Care
A significant aspect of pediatric care involves monitoring and guiding the physical, emotional, and social development of children. Pediatricians provide preventive care through regular check-ups, immunizations, and health education for both children and parents. They also play a key role in diagnosing and managing childhood illnesses and injuries, ensuring that children grow up healthy and resilient.
Work Settings and Collaboration
Pediatricians work in a variety of settings, including hospitals, private practices, and pediatric clinics. They often collaborate with other specialists, such as pediatric surgeons, child psychologists, and adolescent medicine experts, to provide comprehensive care tailored to the needs of younger patients.
Nurse Practitioners and Physician Assistants
Roles and Responsibilities
Nurse practitioners (NPs) and physician assistants (PAs) are advanced practice providers who often work in primary care settings, delivering many of the same services as physicians. They are trained to diagnose and treat medical conditions, prescribe medications, and develop treatment plans. Both NPs and PAs often have a specific area of focus, such as family medicine, pediatrics, or geriatrics, and they work under the supervision or in collaboration with a licensed physician.
Training and Certification
Nurse practitioners are registered nurses with advanced education, typically a Master’s or Doctoral degree in nursing, and they hold national certification in their chosen specialty. Physician assistants, on the other hand, complete a rigorous graduate-level program that includes medical and clinical training, and they must pass a certification exam to practice.
Impact on Healthcare Access
NPs and PAs are essential to the healthcare system, especially in primary care. They help expand access to care, particularly in underserved areas or practices with high patient volumes. Their ability to provide comprehensive care, coupled with their collaborative practice with physicians, makes them invaluable in both urban and rural healthcare settings.
Considerations
When deciding which type of doctor to become, understanding the distinctions between these roles in primary care can help guide your choice. Whether you are drawn to the broad scope of family medicine, the adult focus of internal medicine, the specialized care of pediatrics, or the collaborative nature of NPs and PAs, each path offers unique opportunities to make a significant impact on patient care.
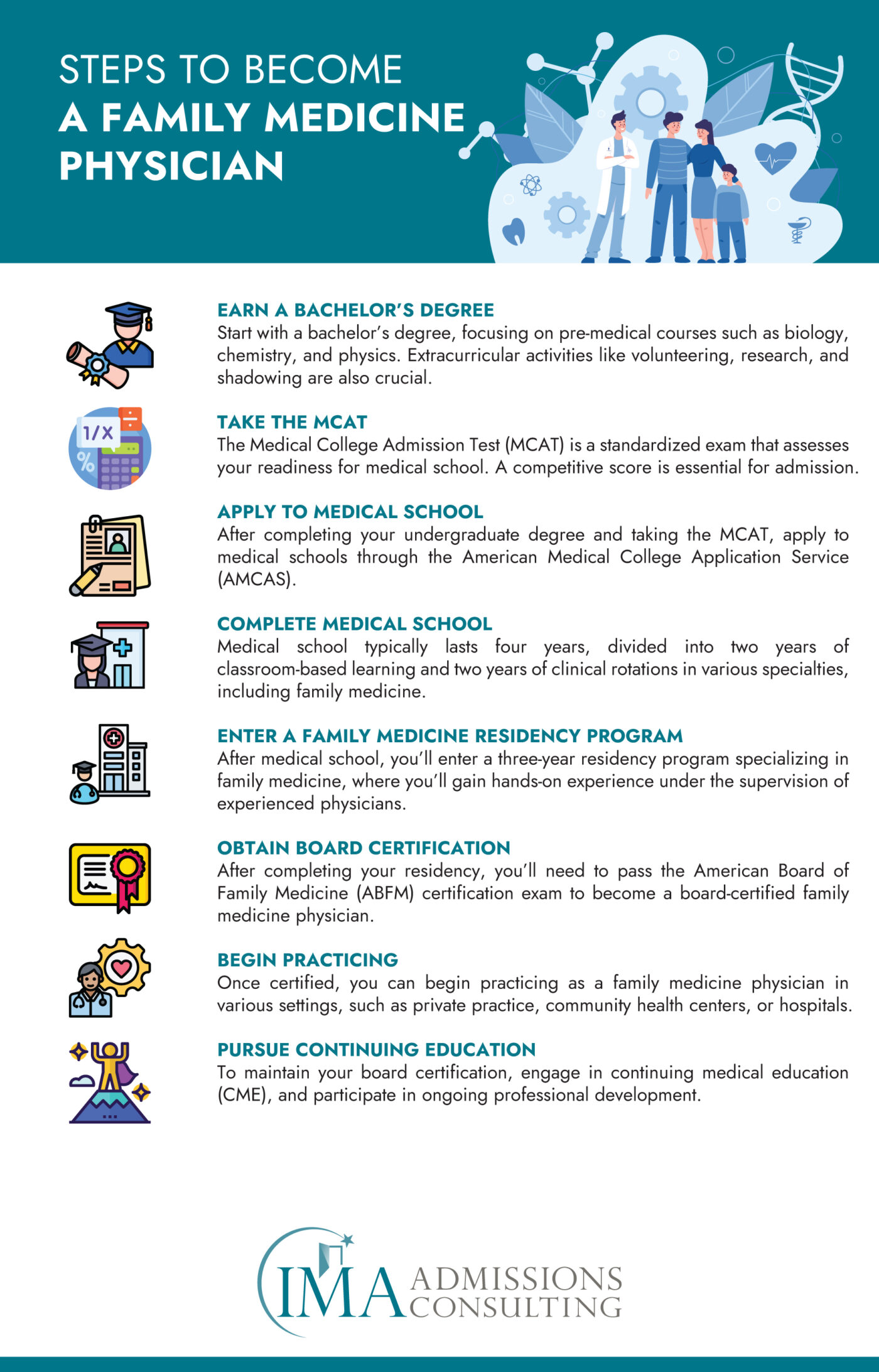
Family Medicine a Closer Look - What is Family Medicine?
Family medicine is a medical specialty that falls under the broader category of primary care. It focuses on providing comprehensive healthcare to individuals across all stages of life, from newborns to the elderly. As a family medicine physician, you are trained to treat a wide variety of health conditions and provide a broad range of services. These services include preventive care, routine check-ups, chronic disease management, and the treatment of acute illnesses. One of the defining characteristics of family medicine is its holistic approach, which often considers the health of the entire family and the various social determinants of health that can affect patient outcomes.
Patient-Centered Care
Family medicine is deeply rooted in patient-centered care, which means that physicians in this field emphasize the importance of understanding the patient within the context of their family and community. This approach enables family physicians to provide more personalized and effective care, as they take into account the patient’s medical history, lifestyle, and social environment when diagnosing and treating conditions.
Long-Term Patient Relationships
Another unique aspect of family medicine is the long-term relationship that physicians often develop with their patients. These ongoing relationships allow family medicine doctors to better understand their patients’ evolving healthcare needs over time, making them well-suited to provide continuous and coordinated care throughout a patient’s life.
Scope of Practice in Family Medicine
Preventive Care
One of the primary responsibilities of family medicine physicians is providing preventive care. This includes conducting routine health screenings, administering immunizations, and performing wellness exams. Preventive care is essential for early detection of health issues and for promoting healthy lifestyle choices among patients. Family physicians also provide counseling on diet, exercise, and other lifestyle factors that can prevent diseases and improve overall health.
Chronic Disease Management
Family medicine physicians are also well-equipped to manage chronic diseases. They often provide long-term care for conditions such as diabetes, hypertension, and asthma. Managing chronic diseases involves regular monitoring, adjusting treatment plans as needed, and educating patients on how to manage their conditions effectively at home. This aspect of family medicine requires a deep understanding of various medical conditions and the ability to work closely with patients to help them maintain their health over the long term.
Acute Care
In addition to managing chronic conditions, family medicine physicians also treat acute illnesses and injuries. This can range from common infections, like the flu, to minor injuries, such as sprains and cuts. Family physicians are often the first point of contact for patients experiencing sudden health issues, and they play a crucial role in diagnosing, treating, and coordinating care if specialized treatment is necessary.
Health Counseling
Beyond physical health, family medicine physicians also provide counseling on a wide range of health-related topics. This includes guidance on mental health, stress management, family planning, and nutrition. Family physicians are trained to address the overall well-being of their patients, recognizing that mental and emotional health are integral parts of a person’s overall health. They often work with patients to develop personalized plans to improve their health and quality of life.
Comprehensive Care Across the Lifespan
Family medicine is unique in its ability to provide continuous care throughout a patient’s life. From infancy through old age, family physicians are equipped to handle a wide array of health issues. This continuity of care is a hallmark of family medicine and provides a strong foundation for maintaining long-term health and well-being.
The Value of Family Medicine
Family medicine is a dynamic and rewarding field that offers the opportunity to provide comprehensive care to a diverse patient population. With a focus on holistic, patient-centered care, family medicine physicians play a crucial role in the healthcare system by addressing a wide range of health issues, from preventive care to the management of chronic diseases. Their ability to develop long-term relationships with patients and their families allows them to deliver continuous and coordinated care, making them an integral part of their patients’ lives and communities.
Comparing Primary Care and Family Medicine
When deciding between a career in primary care and family medicine, it’s crucial to understand the distinctions and overlaps between these two paths. Primary care is an overarching term that includes several medical specialties dedicated to general health care. These specialties include family medicine, internal medicine, pediatrics, and sometimes even obstetrics and gynecology. Primary care physicians serve as the first point of contact for patients, offering comprehensive and continuous care, often coordinating with specialists when necessary.
Family medicine, however, is a specific specialty within primary care. Family physicians are trained to provide comprehensive health care to patients of all ages and genders, treating a wide variety of conditions. They focus on the health of the entire family unit, often considering the social and community contexts that affect their patients’ health. Family medicine is characterized by its broad scope, allowing physicians to address a vast array of health issues across all stages of life.
Key Differences Between Primary Care and Family Medicine
Scope of Care
One of the primary differences between primary care and family medicine lies in the scope of care provided. Primary care encompasses a range of specialties that focus on general health care, including family medicine, internal medicine, and pediatrics. Family medicine specifically, however, is dedicated to providing comprehensive care to individuals across the entire lifespan—from newborns to the elderly. Family physicians are trained to manage a wide array of health issues within the context of the family and community.
In contrast, other primary care specialties like internal medicine or pediatrics have a more focused scope. Internal medicine physicians, for example, concentrate on adult patients, providing care for a wide range of adult health issues but with less emphasis on pediatric or obstetric care. Pediatricians, on the other hand, specialize in the health of children from birth through adolescence. While these specialties fall under the primary care umbrella, they do not offer the same breadth of care across all age groups that family medicine does.
Training Focus
The training for family medicine and other primary care specialties reflects their different scopes of practice. Family medicine physicians undergo a diverse training program that includes rotations in pediatrics, internal medicine, obstetrics and gynecology, geriatrics, and more. This broad training prepares family physicians to provide a wide spectrum of care, making them versatile and capable of treating patients of any age and managing a variety of health conditions.
In comparison, other primary care physicians, such as internists and pediatricians, receive more focused training. Internists are trained specifically in adult medicine, delving deeply into the diagnosis, treatment, and prevention of adult diseases. Pediatricians, meanwhile, focus their training on the health and development of children. While both of these specialties provide essential primary care services, they are more specialized in their patient populations than family medicine physicians.
Patient Population
Another key difference is the patient population each specialty serves. Family medicine physicians care for patients across the entire lifespan, from newborns to seniors. This allows them to treat multiple generations within the same family, providing a continuity of care that can be particularly beneficial for managing chronic conditions and understanding family health histories.
In contrast, other primary care specialties target specific age groups. Pediatricians exclusively treat children and adolescents, focusing on the unique health needs of younger patients. Internists, meanwhile, specialize in adult care, addressing health issues specific to adulthood. While both pediatricians and internists provide primary care, their focus on particular age groups differentiates them from the more all-encompassing practice of family medicine.
Similarities Between Primary Care and Family Medicine
Patient Relationships
Despite the differences in scope and training, both primary care and family medicine emphasize the importance of building strong, long-term relationships with patients. This relationship is central to the practice of both fields, as it fosters continuity of care and allows physicians to gain a deep understanding of their patients’ health histories, lifestyle choices, and personal health goals. Whether a physician is practicing family medicine, internal medicine, or pediatrics, the goal is to provide care that is not only medically effective but also tailored to the unique needs of each patient.
Preventive Health Focus
Both primary care and family medicine prioritize preventive health care. Physicians in both fields work to identify health issues early, manage risk factors, and promote healthy lifestyle choices that can prevent the onset of chronic diseases. This proactive approach to health care is designed to maintain wellness and prevent illness, rather than just treating conditions as they arise. By focusing on preventive care, both primary care and family medicine physicians play a crucial role in promoting long-term health and well-being for their patients.
Comprehensive Care
Another significant similarity between primary care and family medicine is the comprehensive nature of the care provided. Physicians in these fields are often the first point of contact for patients, responsible for addressing a wide variety of health concerns. This includes everything from acute illnesses to chronic disease management, mental health care, and lifestyle counseling. The holistic approach adopted by both primary care and family medicine ensures that patients receive well-rounded care that addresses their physical, emotional, and social health needs.
Choosing Between Primary Care and Family Medicine
When choosing between primary care and family medicine, it’s important to consider your interest in serving specific patient populations versus providing care to a broad range of patients across all ages. While primary care encompasses a variety of specialties, family medicine offers a unique opportunity to provide comprehensive, continuous care within the context of the family and community. Both paths offer the chance to build meaningful relationships with patients and make a significant impact on their health and well-being.
Deciding Your Path and Which Type of Doctor Should You Be?
As you consider whether to pursue a career in primary care or family medicine, reflect on your interests and strengths. If you are drawn to treating a diverse patient population, including children and the elderly, and enjoy the idea of being a continuous presence in your patients’ lives, family medicine may be the ideal choice. This specialty allows for flexibility and variety in your practice, with the opportunity to develop long-term relationships with patients and their families.
Alternatively, if you are more interested in focusing on a specific patient demographic, such as adults or children, or if you prefer working in a particular medical area, such as internal medicine or pediatrics, a broader primary care path might be more suitable. This route allows you to specialize while still providing comprehensive care within your chosen focus area.
Building a Competitive Edge with International Medical Aid (IMA)
Demonstrating Commitment to Service and Global Health
Participation in IMA’s Global Health Internships shows admissions committees that you are committed to serving underserved populations and addressing global health challenges. This commitment aligns with the values of many medical schools that emphasize the importance of service and social responsibility in healthcare. By engaging in meaningful community work, you demonstrate that you are not only interested in the science of medicine but also in its application to improve lives globally.
Developing Cultural Competence
Cultural competence is increasingly recognized as an essential skill for healthcare professionals. Through IMA’s Internships, you gain firsthand experience in diverse cultural settings, learning to provide healthcare in different cultural and socio-economic environments. This experience is highly valued by medical schools, as it prepares you to work effectively with diverse patient populations, an important aspect of modern medical practice.
Gaining Insight into Various Medical Specialties
Shadowing physicians in different specialties through IMA’s programs allows you to explore various fields of medicine. This exposure can help clarify your interests and inform your decision on which specialty to pursue. Medical schools appreciate applicants who have explored different areas of medicine and can articulate their reasons for choosing a particular path. It shows that you have a well-rounded understanding of the medical profession and are making informed career choices.
Enhancing Clinical Skills and Professionalism
Hands-on clinical experience is invaluable for developing the practical skills necessary for medical school and beyond. Through IMA’s internships, you not only observe but also participate in patient care, helping you build confidence and competence in a clinical setting. This experience fosters professionalism, teaches you how to interact with patients and healthcare teams, and provides a solid foundation in the basics of medical practice. These are key attributes that medical schools look for in applicants.
Crafting a Compelling Personal Statement
The experiences you gain through IMA’s internships provide rich material for your personal statement and secondary application essays. You can draw on your clinical experiences, interactions with patients, and insights gained from working in diverse settings to craft a compelling narrative that reflects your commitment to medicine. This narrative can set you apart from other applicants, showing that you have not only academic readiness but also the experiential foundation and personal drive to succeed in medical school.
Networking and Mentorship Opportunities
IMA’s programs connect you with experienced healthcare professionals who can provide mentorship and guidance. Building these relationships can be beneficial as you navigate the medical school application process and your future career. Mentors can offer advice, write strong letters of recommendation, and provide insights into the medical profession that can help you make informed decisions about your career path.
Frequently Asked Questions (FAQ) Section
Choosing a medical specialty can be a complex and challenging decision, especially when considering the nuances between different fields. In this section, we address some of the most common questions and concerns that prospective medical students and healthcare professionals may have about the differences and similarities between family medicine, primary care, and internal medicine. These answers are designed to provide clarity and guidance to make informed decisions about your future career.
What is the difference between family medicine and primary care?
The terms family medicine vs primary care often cause confusion, as they are sometimes used interchangeably. However, family medicine is a specialty within primary care that focuses on providing comprehensive health care to individuals of all ages. Primary care is a broader category that includes not only family medicine but also specialties like internal medicine, pediatrics, and sometimes obstetrics and gynecology. Essentially, while all family medicine physicians are primary care physicians, not all primary care physicians are family medicine doctors.
How do I choose between primary care and family medicine as a career?
Choosing between a career in primary care vs family medicine depends on your interests and career goals. If you enjoy providing comprehensive care to patients of all ages and forming long-term relationships with families, family medicine might be the right path for you. On the other hand, primary care encompasses a wider range of specialties, allowing you to focus on specific patient populations, such as adults in internal medicine. Understanding the scope and patient demographics you wish to serve can help you decide.
What are the similarities between internal medicine, family medicine, and primary care?
When comparing internal medicine vs family medicine vs primary care, it’s important to recognize the overlaps in their roles. All three focus on providing comprehensive care, but their patient demographics and training differ. Internal medicine doctors specialize in adult care, family medicine covers all ages, and primary care serves as an umbrella term that includes both specialties. These fields share a commitment to preventive care, managing chronic diseases, and providing ongoing patient support.
What is a primary care physician vs family medicine doctor?
The distinction between a primary care physician vs family medicine doctor lies in the scope of practice. A primary care physician could be a doctor specializing in family medicine, internal medicine, or pediatrics, providing first-contact care and managing overall patient health. A family medicine doctor specifically is trained to care for patients across all age groups, making them a versatile choice within the primary care category. This training enables them to treat a wide range of conditions, from pediatrics to geriatrics, under the primary care umbrella.
Why is understanding family medicine vs primary care important for medical students?
Understanding the difference between what is family medicine vs primary care for medical students can help them decide on their career path. While both offer rewarding opportunities in patient care, knowing the distinctions can guide students in choosing a specialty that aligns with their interests. Family medicine offers the chance to treat a diverse patient population, often within the context of a family, while primary care allows for specialization in areas like internal medicine, focusing more on adults or other specific groups. This clarity helps students make informed decisions about their future roles in healthcare.
Closing Thoughts
Choosing between primary care and family medicine is a significant decision that will shape your career as a physician. Both paths offer the opportunity to make a profound impact on patients’ lives, whether through the broad reach of primary care or the specialized, holistic approach of family medicine. By understanding the differences and similarities between these fields, you can make an informed decision that aligns with your career goals and personal passions.





