SOAP—Subjective, Objective, Assessment, Plan—is a standardized framework for documenting patient encounters during clinical rotations. It streamlines how you collect, organize, and present data, ensuring you can track symptoms to their likely causes efficiently. For medical students, mastering SOAP it’s about proving you can think and communicate like a clinician, a skill that pays off in rounds, medical school applications, and global healthcare internships.
Most hospitals use electronic systems formatted in SOAP but don’t rely on them alone. Carry a notebook and pen—software access can lag when you’re juggling patients and tasks. Being prepared keeps you sharp and independent.
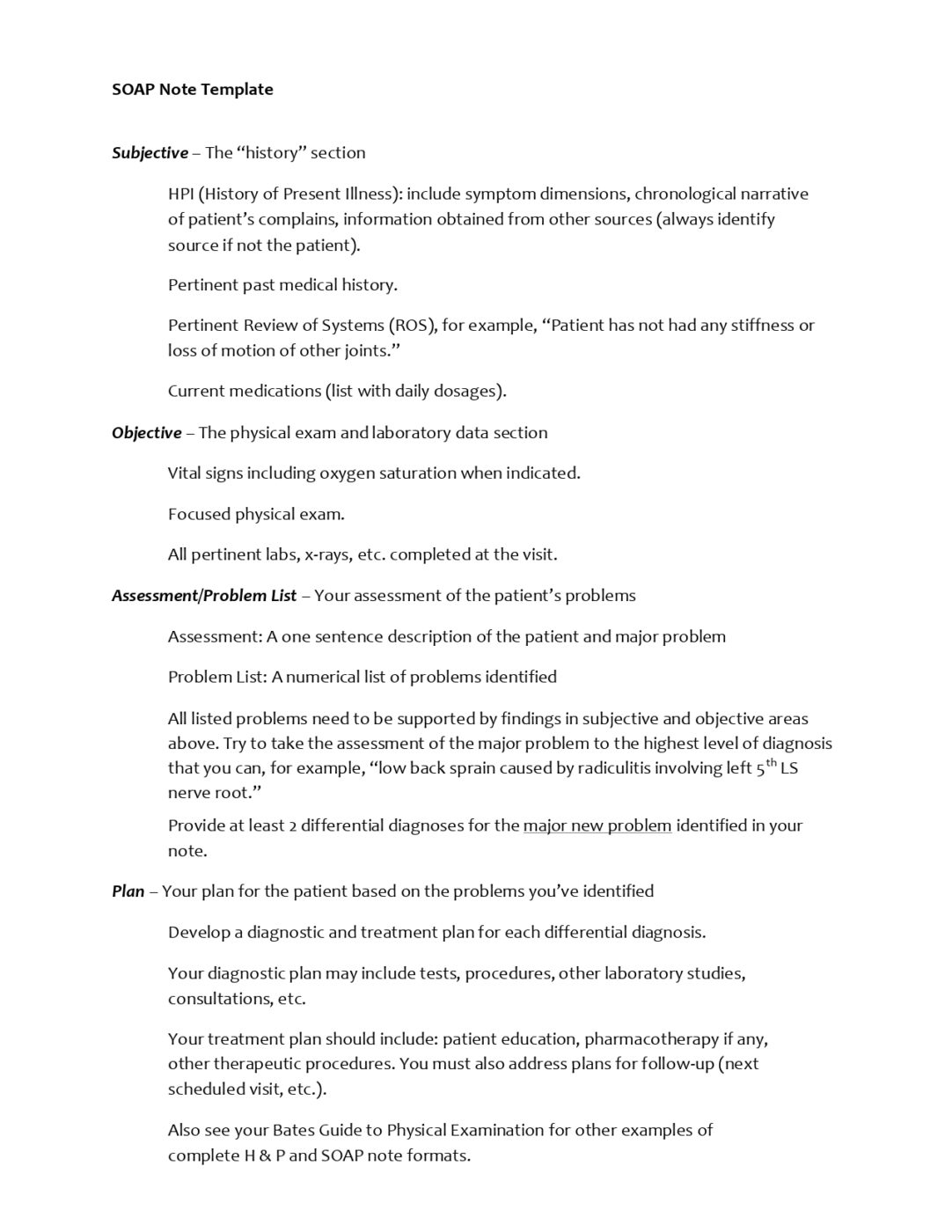
Subjective: Start with the Patient’s Story
The Subjective section captures what the patient tells you—unmeasurable but foundational. It’s their raw input: complaints, history, sensations. Take two patients who’ve lost equal blood from a cut. One says “a little,” the other “a lot.” That’s subjective—perception varies. Use the OLDCHARTS mnemonic to structure it:
- Onset: When did symptoms start? A timeline narrows the cause.
- Location: Where’s the issue—pain, rash, whatever? Pinpoint it.
- Duration: How long has it been going on? Duration refines the context.
- Character: What’s it like—sharp, dull, burning? Details matter.
- History: What’s the patient’s past medical background? History shapes the narrative.
- Alleviating Factors: Does anything ease it—rest, movement? This hints at mechanisms.
- Radiation: Does it spread from chest to arm, back to leg? Patterns inform causality.
- Temporal Patterns: Constant or intermittent? Timing reveals triggers.
- Symptoms Associated: Any extras—nausea with pain? Completes the picture.
Ask focused questions. Record precisely. This isn’t chit-chat—it’s data collection.
Objective: Ground It in Evidence
Next, Objective: what you observe and measure. Pulse, blood pressure, respiration, swelling, cuts—anything tangible. It goes here if you see, hear, or test it. Don’t guess at a diagnosis yet. Just list the facts. A patient with a fever and rapid breathing? Note the numbers and signs, not “probably pneumonia.” Accuracy here builds trust in your assessments later.
Assessment: Connect the Dots
Assessment fuses Subjective and Objective into a working diagnosis. A patient reports abdominal pain (Subjective), and you find tenderness on the exam (Objective)—maybe appendicitis, gastritis, or a blockage. Some cases are obvious. Others demand you sift through overlapping symptoms. Go with the most probable cause based on what you’ve got. New data might shift it later—stay flexible.
Plan: Act and Communicate
The Plan turns your assessment into action. Antibiotics for an infection? Imaging for uncertainty? List what’s next and why. If it’s a test, say what you’re ruling out. If it’s treatment, tie it to the diagnosis. Don’t leave patients guessing—explain the steps clearly. A confused patient is a stressed patient, which you must avoid.
Keep Your Notes Tight
Disorganized SOAP notes tank your performance in rounds. Sort them by date, severity, or duration—not just the order you scribbled them. A patient with a chronic cough comes up. You’ll flip straight to it, not fumble. Adapt the system to your brain, but keep it consistent. Precision here signals competence.
Handle the Pressure
Rounds are intense—forgetting details or stumbling can rattle you. No one expects perfection early on; mentors will catch your slip-ups and guide you. The fix isn’t gimmicks—it’s preparation. Review your notes nightly. Sleep enough. Exhaustion breeds errors, and patients deserve better. Stress fades when you’re ready.
Leveraging SOAP Notes to Build Clinical Reasoning Skills
As a medical student aspiring to excel in clinical rotations and secure a spot in medical school, mastering the SOAP format is more than just a note-taking exercise—it’s a gateway to developing clinical reasoning skills that will set you apart. Clinical reasoning is the ability to analyze patient data, connect the dots between symptoms and causes, and make informed decisions. It’s a skill medical schools and residency programs highly value, and SOAP notes provide a structured framework to hone it early on. Here’s how you can leverage SOAP to build this critical competency:
Practice Hypothesis-Driven Thinking
In the Subjective and Objective sections, you gather raw data—patient complaints, vital signs, and physical exam findings. Use this as an opportunity to start forming hypotheses. For example, if a patient reports chest pain (subjective) and you observe an elevated heart rate (objective), ask yourself: What could this be? Cardiac-related? Respiratory? Anxiety-driven? Don’t jump to conclusions, but let these questions guide your note-taking. This habit trains your brain to think critically from the outset, a skill that will shine in medical school interviews and clinical discussions.
Strengthen Differential Diagnosis in the Assessment
The Assessment section is where your clinical reasoning takes shape. Instead of settling on a single diagnosis, challenge yourself to list at least three potential differential diagnoses based on the subjective and objective data. For instance, if a patient has a fever, cough, and fatigue, your differentials might include pneumonia, bronchitis, or even early viral sepsis. Briefly note why each is plausible and what additional information (e.g., a chest X-ray or lab results) would confirm or rule them out. This exercise mirrors how seasoned physicians think and prepares you for crafting compelling patient presentations during rounds or admissions essays where you showcase your analytical skills.
Link Plans to Evidence
In the Plan section, justify them beyond listing treatments or tests. If you recommend an antibiotic, note that it’s based on a suspected bacterial infection from your assessment. If you order a CT scan, tie it to a differential that needs imaging for confirmation. This practice builds a logical bridge between data and action, reinforcing evidence-based decision-making. Medical schools look for students who think this way, and documenting your reasoning in SOAP notes creates a record you can reflect on to improve.
Reflect and Refine
After completing a SOAP note, take five minutes to review it. Ask yourself: Did I miss any key subjective details? Are my objective findings thorough? Does my assessment align with the data, and is my plan realistic? Reflection turns SOAP into a learning tool, not just a task. Over time, you’ll spot patterns in your thinking—maybe you overlook certain symptoms or rush to a diagnosis too quickly. Correcting these tendencies early will make you a sharper clinician and a standout applicant when discussing patient cases with admissions committees.
Simulate Real-World Scenarios
To take this further, practice SOAP notes outside of rotations. Use case studies from textbooks, online resources, or even hypothetical scenarios you create (e.g., “A 45-year-old male with sudden abdominal pain”). Write a full SOAP note, then compare your assessment and plan to the actual diagnosis if available. This simulation builds confidence and exposes you to diverse conditions, preparing you for the unpredictable nature of clinical work and the rigorous problem-solving demanded in medical school.
Opportunities with International Medical Aid
Explore Hands-On Medical Experience
International Medical Aid offers a transformative program through its Pre-medicine Internships, designed for students and aspiring healthcare professionals eager to gain practical experience in clinical settings. Participants are immersed in global healthcare environments, shadowing doctors, assisting with patient care, and observing medical procedures firsthand. This initiative stands out by providing access to diverse medical practices worldwide, fostering a deeper understanding of how healthcare is delivered across cultures. It’s an ideal stepping stone for those preparing for medical school or a healthcare career, blending real-world exposure with professional development.
Connecting Internship Experience to SOAP Notes
The skills gained in this program align closely with the framework of SOAP notes—Subjective, Objective, Assessment, and Plan—a cornerstone of clinical documentation. Interns witness how healthcare providers collect subjective patient histories, record objective findings like vital signs, assess conditions based on evidence, and devise actionable treatment plans. This direct observation sharpens their ability to understand and eventually craft SOAP notes themselves, translating internship experiences into a practical tool for organizing patient information. By engaging in such immersive learning, participants build a foundation that enhances their clinical competence and readiness to apply structured documentation in future practice.
By treating SOAP notes as a training ground for clinical reasoning, you’re not just organizing information—you’re building a mindset that will help you shine in medical school applications and thrive during global healthcare internships. Mentors will see your preparedness for hands-on patient care, and admissions officers will recognize your ability to think critically—qualities that International Medical Aid’s consulting and internship programs are designed to highlight and enhance.
Final Thoughts
SOAP is a framework that sharpens your clinical thinking and communication. Nail it early, and it’ll carry you through rotations, impress mentors in global internships, and bolster your medical school apps. Ask a mentor for a sample if you’re stuck, but don’t wait to start. Practice now, and you’re ahead of the pack.





