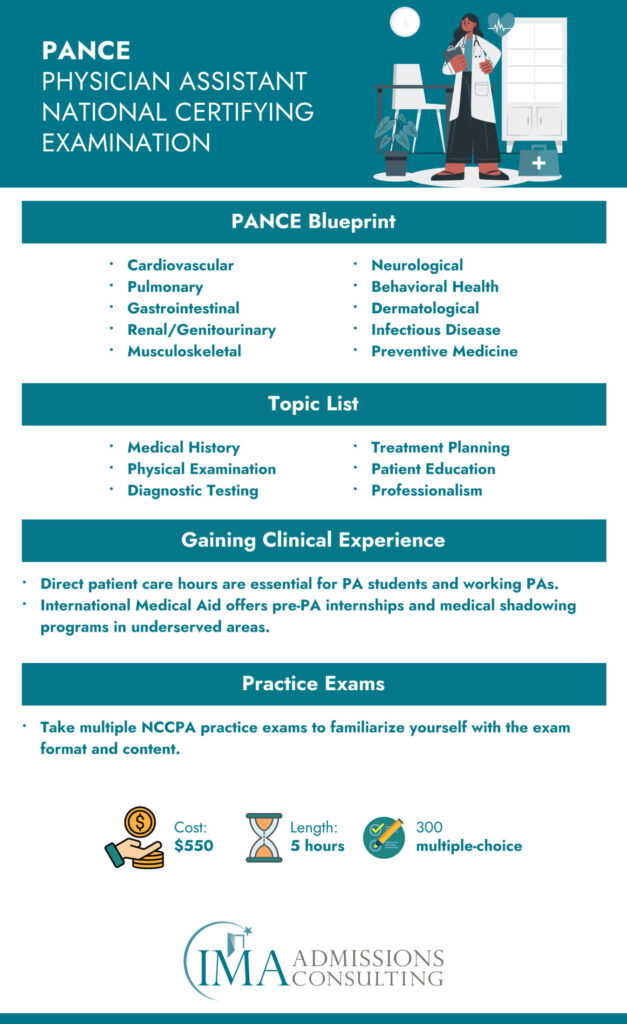
Understanding the PANCE Blueprint
The PANCE blueprint is a foundational document that guides the content and structure of the Physician Assistant National Certifying Exam (PANCE). It provides a comprehensive PANCE topic list encompassing various medical and surgical disciplines a Physician Assistant (PA-C) must master. The PANCE blueprint ensures the exam aligns with current practice and checks a candidate’s readiness to practice healthcare effectively. You can view the blueprint here.
Frequency of PANCE and Key Dates
The PANCE exam is offered multiple times throughout the year, with testing windows typically running from January to December. The 2025 PANCE exam administration window is January 3, 2025, to December 16, 2025. Candidates should register for the exam early to ensure their desired testing date is available.
PANCE Cost and Budgeting
The PANCE exam fee is $550. Candidates should also budget for the cost of travel and accommodations, if necessary. Some PA programs may offer financial assistance to help students cover the cost of the exam.
Duration and Structure of the PANCE
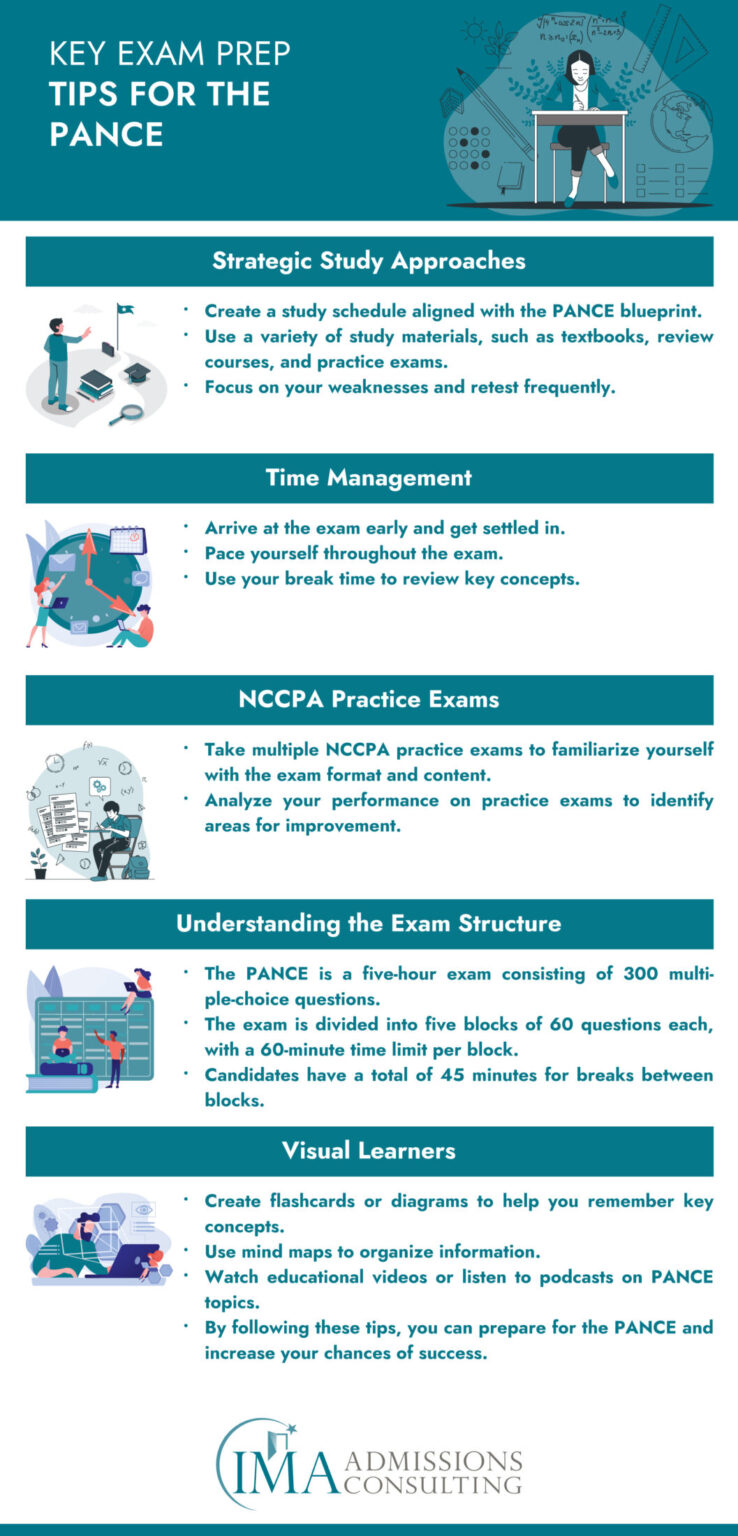
The PANCE exam is a five-hour exam consisting of 300 multiple-choice questions. The exam is divided into five blocks of 60 questions each, with a 60-minute time limit per block. Candidates have a total of 45 minutes for breaks between blocks.
NCCPA Practice Exam as a Preparation Tool
Utilizing the NCCPA practice exam is an excellent way to prepare for the PANCE. These practice exams mimic the actual test’s structure and content, offering candidates a realistic insight into their preparedness for the PANCE.
Gaining Clinical Experience
Direct patient care hours are essential for PA students, not only for admissions but as practical experience that underpins theoretical knowledge. Physician Assistant Internships Abroad can offer invaluable experience and exposure to diverse medical practices. Moreover, how to gain direct patient care hours should be a primary focus for those looking to apply their knowledge in real-world settings.
International Medical Aid offers services to help PA students gain the direct patient care hours they need for admissions and their future careers. These services include:
- Pre-PA internships: International Medical Aid offers pre-PA internships in a variety of countries, including Peru, Kenya and Tanzania. These internships provide students with the opportunity to work alongside experienced medical professionals and gain hands-on experience in a variety of clinical settings.
- Medical shadowing programs: International Medical Aid also offers medical shadowing programs in a variety of specialties, such as family medicine, pediatrics, and surgery. These programs allow students to observe physicians and other healthcare professionals at work and learn about the different aspects of medical practice.
In addition to providing students with direct patient care hours, International Medical Aid programs also offer the following benefits:
- Exposure to diverse medical practices: International Medical Aid programs allow students to experience healthcare delivery in different countries and cultures. This can help students to develop a global perspective on healthcare and learn about different approaches to medical practice.
- Opportunity to work with underserved populations: Many International Medical Aid programs are located in underserved areas, where students have the opportunity to work with patients who may have limited access to healthcare. This experience can help students to develop a strong sense of compassion and commitment to serving their communities.
- Personal and professional development: International Medical Aid programs can also be a valuable personal and professional development experience. Students can challenge themselves, learn new skills, and grow as individuals.
Overall, International Medical Aid programs are a great way for PA students to gain the direct patient care hours they need, as well as exposure to diverse medical practices, the opportunity to work with underserved populations and personal and professional development.
Additionally, the following are some specific examples of how International Medical Aid programs can help PA students gain direct patient care hours:
- Pre-PA interns at International Medical Aid intern in a variety of clinical settings, such as hospitals, clinics, and rural health centers. They may have the opportunity to assist with tasks such as taking patient vitals, performing physical exams, and administering medications.
- Medical shadowing students at International Medical Aid typically follow physician assistants or other healthcare professionals for a set number of hours per day or week. They observe the healthcare professional during patient appointments, surgeries, and other procedures.
By participating in an International Medical Aid program, PA students can gain the direct patient care hours they need for admissions and their future careers, while also experiencing a rewarding and educational opportunity.
PA School Admissions and Guidance
Embarking on the journey to become a certified Physician Assistant (PA-C) is an ambitious and rewarding endeavor. The PANCE, or Physician Assistant National Certifying Exam, is a vital stepping stone on this path. This extensive examination assesses the medical knowledge and clinical skills of PA candidates, ensuring readiness for professional practice.
A deep understanding of the PANCE blueprint is critical for candidates as it details the scope and various medical topics that the exam covers. In preparing for the PANCE, it is beneficial to engage with the NCCPA Practice Exam several times. These practice assessments are designed to emulate the structure and content of the actual PANCE and are invaluable for honing test-taking strategies.
The PANCE topic list is another crucial resource that outlines the content domains of the exam. Familiarity with this list will guide your study sessions and ensure comprehensive coverage of all necessary subjects.
It’s also practical to be aware of the number of questions on the PANCE and the time allotted for the exam. The PANCE consists of 300 questions and spans five hours, requiring focused preparation to build up the endurance and speed needed.
Knowledge of PANCE Exam Dates 2025 is essential for scheduling and planning your study regimen. Aligning your preparation with the PANCE schedule ensures you are well-prepared when the test day arrives.
The cost of the PANCE is also a point of consideration. Investing in this exam goes beyond the financial aspect; it also encompasses the dedication of your time and effort to succeed.
Beyond the exam, engaging in Physician Assistant Internships Abroad can offer a broadened perspective on healthcare practices in different cultural contexts. Additionally, accruing direct patient care hours is a critical component of PANCE eligibility and invaluable to your clinical acumen.
For individualized support, PA School Admissions Consulting services can provide tailored advice and strategic planning assistance to help you navigate through the complexities of the admissions process.
With your sights set on conquering the PANCE and advancing toward a career as a PA-C, it is important to immerse yourself in the study materials and resources available to ensure success on the exam and beyond.
The PANCE Examination Blueprint a Guide for Aspiring Physician Assistants
In 2019, the Physician Assistant National Certifying Examination (PANCE) underwent a significant revision in its content blueprint. This change was designed to provide more specific guidance to Physician Assistant (PA) candidates preparing for this crucial assessment. The PANCE serves as a comprehensive and rigorous evaluation of the knowledge and skills that are essential for PAs entering the field.
Structure and Components of the PANCE Blueprint
The updated PANCE blueprint aligns the examination with two principal dimensions:
- Medical Knowledge: This dimension focuses on the diseases and disorders PAs are likely to encounter in practice.
- Clinical Skills: This dimension assesses the practical tasks and responsibilities PAs perform in patient care.
These dimensions are expansive, ensuring a well-rounded examination of a candidate’s capabilities.
Understanding the Content Categories
The blueprint provides detailed listings under each category, exemplifying potential exam material. However, due to the extensive scope of medical knowledge, not all topics can be covered in a single examination session, and occasionally, questions may address content beyond the provided examples.
The Role of Certified Physician Assistants in Shaping the PANCE
The development and ongoing refinement of the PANCE blueprint is a collaborative effort involving certified PAs. These professionals participate in practice analysis studies and are integral to the exam question development process, ensuring the relevance and currency of the content as medical practices evolve.
Medical Content Categories and Their Allocation
Each medical content category is assigned a specific percentage of the examination, reflecting its importance and frequency in PA practice:
- Cardiovascular System: 13%
- Dermatologic System: 5%
- Endocrine System: 7%
- Eyes, Ears, Nose, and Throat: 7%
- Gastrointestinal System/Nutrition: 9%
- Genitourinary System (Male and Female): 5%
- Hematologic System: 5%
- Infectious Diseases: 6%
- Musculoskeletal System: 8%
- Neurologic System: 7%
- Psychiatry/Behavioral Science: 6%
- Pulmonary System: 10%
- Renal System: 5%
- Reproductive System (Male and Female): 7%
Task Categories and Their Allocation
The PANCE also evaluates various task categories associated with the PA profession, such as:
- History Taking and Physical Examination: 17%
- Diagnostic and Laboratory Studies: 12%
- Formulating Most Likely Diagnosis: 18%
- Patient Management and Preventive Measures: 10%
- Clinical Intervention: 14%
- Pharmaceutical Therapeutics: 14%
- Applying Basic Scientific Concepts: 10%
- Professional Practice: 5%
Up to 20% of the exam may cover general surgical topics, with slight variations in the percentage allocations.
Emphasis on Sample Questions and Resources
The National Commission on Certification of Physician Assistants (NCCPA) recognizes the importance of practice and familiarity with exam structure for candidates. To aid in this, the NCCPA has provided sample questions that are retired from the active item pool.
For those preparing for the PANCE, reviewing these sample questions is invaluable for understanding the level of complexity and the reasoning required for the actual examination. Detailed critiques from the NCCPA test committee accompany these questions, elucidating why certain answers are correct and why others are not.
Utilizing the NCCPA's Resources
In conjunction with our resources, we strongly recommend visiting the NCCPA’s official website to explore additional sample questions. This will broaden your exposure to the variety of question formats and content areas on the PANCE. You can access these valuable resources here: Sample Questions.
Maximizing Your PA Application Through Global Internships and Admissions Consulting
In today’s competitive Physician Assistant (PA) landscape, securing a standout application means combining academic achievement with hands-on clinical experience and tailored admissions guidance. International Medical Aid (IMA) offers unique global internship programs along with specialized admissions consulting designed to help you build a strong, well-rounded application. This section introduces innovative strategies to leverage IMA’s offerings, with direct links to learn more about our programs, our process, and our success stories.
Global Internships: Real-World Clinical Experience Abroad
Gain Practical Experience in Diverse Healthcare Environments
IMA’s global internship programs provide you with the opportunity to work in a variety of clinical settings in countries known for their diverse healthcare challenges. Whether you are assisting in community clinics or observing patient care in busy hospitals, these internships allow you to experience firsthand how healthcare is delivered in different parts of the world. This hands-on experience enriches your understanding of clinical practices and helps you develop practical skills that are critical for a successful PA career.
- Diverse Clinical Settings: International Medical Aid partners with healthcare institutions in regions such as South America, Africa, and Asia. These placements expose you to different patient populations, healthcare delivery methods, and resource management techniques.
- Real-World Application: By participating in these internships, you get the chance to perform tasks such as taking patient vitals, assisting with physical examinations, and learning about diagnostic procedures. These real-world experiences reinforce what you learn in the classroom and demonstrate your commitment to patient care.
To learn more about our internship opportunities, please visit our Pre-Med Internships page.
Develop Cultural Competence and Clinical Insight
Working abroad not only hones your clinical abilities but also helps you build cultural competence. Exposure to different healthcare systems and patient backgrounds enables you to appreciate how social, economic, and cultural factors influence patient care. This understanding is a valuable asset in PA school applications and clinical practice, as it shows you can adapt to diverse environments and effectively communicate with patients from various backgrounds.
- Cultural Exchange: Interacting with healthcare professionals and patients in international settings broadens your perspective and allows you to see challenges and solutions that may be uncommon in domestic settings.
- Building a Global Network: Through these internships, you will establish professional relationships that can lead to future mentorship and collaboration opportunities. These connections are essential for your career growth and can provide long-term support as you progress through your PA journey.
Admissions Consulting: Tailored Support to Enhance Your Application
Personalized Guidance for Crafting a Standout Application
In addition to gaining practical experience, presenting your accomplishments through a polished and persuasive application is key. IMA’s admissions consulting services offer personalized support to help you navigate the PA school admissions process from start to finish.
- Application Review and Strategy: Our experienced consultants work with you to review your application materials. They help you refine your personal statement and secondary essays so that your narrative effectively highlights both your academic achievements and your clinical experiences abroad.
- Interview Preparation: A critical part of the admissions process is the interview. IMA’s consulting services include mock interviews, providing you with the opportunity to practice and receive feedback. This preparation ensures you can confidently share your experiences and answer questions about your global internship and clinical exposure.
- Timely Deadline Management: Navigating multiple application deadlines can be overwhelming. Our team provides strategic planning to ensure you meet all key dates, allowing you to submit a complete and timely application.
For a detailed explanation of our consulting process and to see how it works, visit our How It Works page.
Leveraging International Experience in Your Application
One of the most powerful aspects of IMA’s offerings is the integration of global internships with admissions consulting. The practical experiences you gain abroad serve as compelling content for your application, demonstrating that you have a well-rounded background and the ability to thrive in diverse clinical environments.
- Developing a Unique Narrative: Global internship experiences provide concrete examples that can distinguish your application. Whether it’s a case where you learned an innovative approach to patient care or observed a unique healthcare challenge, these stories enrich your personal statement and interview responses.
- Showcasing Your Adaptability: Admissions committees value candidates who can adapt to different settings and overcome challenges. By highlighting your international experience, you underscore your adaptability and commitment to learning, qualities that are essential for a future PA.
- Demonstrating Commitment: Your decision to pursue an internship abroad indicates a proactive approach to education and a genuine interest in global health issues. This commitment is a strong indicator of your potential to contribute positively to the healthcare community.
To see firsthand how our programs have impacted others, check out our Alumni Testimonials. These success stories offer insights into how previous candidates have leveraged their international experiences to gain admission into top PA programs and succeed in their careers.
Integrating Internships and Consulting for a Competitive Edge
Combining Practical Experience with Strategic Guidance
The integration of global internships and admissions consulting creates a powerful, synergistic approach to your PA journey. With real-world clinical experience enhancing your application narrative, and personalized consulting ensuring that every detail of your application is optimized, you gain a significant advantage over other candidates.
- Holistic Application Development: The practical knowledge and cultural insights from your global internship provide rich material for your application. With expert guidance, you can articulate these experiences in a way that highlights your readiness for a challenging clinical environment.
- Enhanced Interview Performance: When it comes time to interview, you will have a reservoir of real-world examples to draw upon. Our consultants help you prepare by refining your responses and ensuring that you can clearly communicate your experiences and insights.
- Strategic Use of Resources: Both global internships and admissions consulting are designed to complement one another. While internships give you the practical skills and experiences, consulting services help you strategically incorporate these elements into your application. This coordinated approach makes your profile not only robust but also compelling.
Next Steps: Get Started with IMA
If you’re ready to strengthen your PA application and gain invaluable international clinical experience, consider taking advantage of International Medical Aid’s offerings. Visit our Pre-Med Internships page for detailed information on available programs, locations, and program fees. To learn more about how our process works, check out the How It Works page, and don’t miss out on the success stories shared by past participants on our Alumni Testimonials page.
By combining global clinical experiences with tailored admissions consulting, International Medical Aid provides a comprehensive solution to help you build a competitive PA application. This integrated approach not only enhances your clinical skills but also ensures that your application stands out with a unique narrative, strong recommendations, and well-prepared interview performance. Embrace these opportunities to transform your educational journey and move one step closer to a rewarding career as a Physician Assistant.
Preparing for Success
The PANCE is a pivotal milestone in the journey to becoming a certified PA. The updated content blueprint and the availability of sample questions are instrumental in guiding your study strategy. By comprehensively understanding the exam’s structure and engaging with practice questions, you can approach your test day with confidence, equipped with the knowledge and skills necessary to succeed.
In the upcoming sections of our guide, we will delve into the specifics of our sample questions, providing you with a robust preparation tool designed to complement the official materials provided by the NCCPA. Let’s embark on this journey to ensure your success on the PANCE.
Sample PANCE Questions
Building on the foundation laid by the NCCPA’s resources, our guide offers an extensive array of sample questions tailored to mirror the updated PANCE blueprint. These questions are constructed to challenge and enhance your critical thinking and problem-solving abilities in a manner consistent with the actual examination.
Our sample questions section serves as a practical tool to assess your readiness and to familiarize yourself with the types of questions you may encounter. Through active engagement with these practice items, candidates can identify areas of strength and pinpoint topics that may require further review.
A 55-year-old female presents with progressive exertional dyspnea over the past two months and intermittent bilateral lower extremity edema. She has a history of hypertension and hyperlipidemia. On physical examination, her blood pressure is 145/90 mmHg, and there is 2+ pitting edema in both ankles. Lung auscultation reveals bibasilar crackles. A chest X-ray shows an enlarged cardiac silhouette and pulmonary congestion. Her ECG indicates left ventricular hypertrophy.
Which is the most appropriate next step in managing this patient?
A. Initiate furosemide therapy
B. Perform a coronary angiography
C. Start beta-blocker therapy
D. Arrange for an immediate heart transplant evaluation
E. Prescribe an ACE inhibitor
Critique: This question assesses the examinee’s ability to determine the next step in managing a patient with signs and symptoms suggestive of heart failure.
Option (A), initiate furosemide therapy, is correct because it will address the fluid overload evidenced by the patient’s dyspnea, edema, and pulmonary congestion.
Option (E), prescribing an ACE inhibitor, is also a correct management strategy in chronic heart failure, particularly for long-term management to improve survival, but the immediate concern is to relieve symptoms caused by fluid retention.
Option (B), performing a coronary angiography, would be considered if there were evidence of ischemic heart disease, but this patient’s presentation is more consistent with heart failure.
Option (C), starting beta-blocker therapy, is a part of the long-term management of heart failure but is not indicated as an immediate step before addressing the volume overload.
Option (D), arranging for an immediate heart transplant evaluation, is premature and would only be considered in end-stage heart failure unresponsive to medical therapy.
A 62-year-old woman with a history of type 2 diabetes mellitus presents with complaints of progressive fatigue and intermittent claudication. Her pulse is weak in the left lower extremity. A bruit is auscultated over the left femoral artery. Ankle-brachial index on the left is 0.65. Based on the PANCE blueprint, which of the following is the most appropriate initial management for this patient?
A. Start a trial of cilostazol.
B. Refer for immediate vascular surgery consultation.
C. Schedule for percutaneous transluminal angioplasty.
D. Prescribe an antiplatelet agent.
E. Initiate high-dose statin therapy.
Critique: This question challenges the examinee’s ability to address peripheral arterial disease (PAD) as detailed in the cardiovascular system section of the PANCE blueprint.
The correct answer is (D): prescribe an antiplatelet agent. The use of antiplatelet therapy, such as aspirin or clopidogrel, is recommended for patients with PAD to reduce the risk of cardiovascular events, as noted 10-100 times in studies related to PANCE preparation.
Option (A), starting a trial of cilostazol, may improve symptoms of claudication, but it does not address the immediate need for cardiovascular risk reduction.
Options (B) and (C), referring for vascular surgery consultation and scheduling for angioplasty, may be necessary if symptoms are severe or if there is a critical limb ischemia, which doesn’t seem to be the case here.
Lastly, while high-dose statin therapy, mentioned in Option (E), is part of the long-term management of atherosclerosis, the immediate need is to reduce thrombotic risk.
A 55-year-old male patient arrives at the clinic complaining of severe pain and a "burning" sensation in his right leg. He describes the pain as sudden in onset and escalating in severity. Upon examination, you observe that the affected leg is pale and notably cooler to the touch compared to the contralateral side. Despite your efforts, you're unable to detect a palpable pulse in the extremity. Given these clinical findings, you consider the potential for an acute vascular event.
Which of the following diagnostic tools is most likely to identify the source of this patient's symptoms in approximately 95% of cases?
A. Chest x-ray
B. Echocardiogram
C. Angiogram
D. Abdominal flat plate
E. Aortic ultrasound
Critique: This PANCE question examines the candidate’s ability to select the appropriate diagnostic modality for a patient presenting with signs suggestive of an acute arterial occlusion. The correct answer is (C), Angiogram.
An angiogram is an imaging test that utilizes contrast material to visualize the arteries. In the scenario described, the patient’s symptoms are consistent with an acute arterial occlusion, and an angiogram is the gold standard for diagnosing this condition. It has a high sensitivity and can identify the obstruction in approximately 95% of cases, making it the diagnostic modality of choice.
Choice (A), Chest x-ray, would not provide information about the arterial flow of the extremity and is therefore not suitable for this clinical presentation.
Choice (B), Echocardiogram, is mainly used for assessing cardiac structure and function and is not indicated for evaluating peripheral artery disease directly.
Choice (D), an abdominal flat plate, is a type of X-ray that can detect issues like bowel obstructions or free air in the abdomen but does not visualize blood vessels and, therefore, would not be useful in this situation.
Lastly, choice (E), Aortic ultrasound, could assess for aortic aneurysms or dissection but would not be the most appropriate test for diagnosing an occlusion in the extremities.
Therefore, the most accurate and definitive choice for diagnosing the source of the extremity pain and burning sensation, given the lack of palpable pulse and the difference in limb temperature, is (C) Angiogram.
A 41-year-old female presents with a constellation of symptoms persisting for nine months, including nausea, constipation, discomfort in the stomach, fatigue, joint pain, and a decline in cognitive function. She reports no significant medical history and maintains a regular menstrual cycle. Upon examination, no notable physical abnormalities are detected. However, laboratory results reveal the following serum levels:
- Albumin: 4.9 g/dL
- Calcium: 13.0 mg/dL (elevated)
- Chloride: 111 mEq/L
- Creatinine: 1.0 mg/dL
- Phosphate: 0.3 mg/dL (decreased)
- Blood urea nitrogen: 17 mg/dL
Given these findings, what is the most probable diagnosis?
A. Cushing syndrome
B. Hyperparathyroidism
C. Hypopituitarism
D. Malabsorption
E. Multiple myeloma
Critique: This PANCE question challenges the test-taker to correlate the patient’s clinical presentation and lab results to pinpoint the underlying disorder.
The correct choice is (B) Hyperparathyroidism. The clinical symptoms align with those associated with hyperparathyroidism, which often presents with musculoskeletal discomfort, gastrointestinal issues, mental changes, and profound fatigue. The key laboratory findings supportive of this diagnosis are the elevated calcium level and reduced phosphate level, both hallmark signs of hyperparathyroidism.
Choice (A), Cushing syndrome, does not fit the clinical picture as it typically manifests with different menstrual patterns and distinctive changes in physical appearance.
Choice (C), Hypopituitarism, is unlikely as the patient lacks the broad spectrum of metabolic, developmental, and reproductive disturbances that would suggest an insufficiency in pituitary hormones.
Choice (D), Malabsorption, is not supported by the patient’s history or laboratory data; symptoms like significant weight loss and other systemic signs are absent.
Lastly, choice (E), Multiple myeloma, typically presents with anemia, bone pain, kidney dysfunction, and protein in the urine, none of which are observed in this patient’s presentation. Moreover, the age demographic for multiple myeloma usually skews older than the patient described here.
A 32-year-old woman arrives with a rapid heart rhythm identified as narrow-complex tachycardia on her 12-lead ECG. Her vitals include a blood pressure of 110/72 mmHg and a pulse of 156 beats per minute. She reports no angina or difficulty breathing. What is the most appropriate next step in management?
A. Bretylium 500 mg IV
B. Verapamil 5 mg IV
C. Adenosine 6 mg IV
D. Digoxin 0.5 mg IV
E. Lidocaine 100 mg IV
Critique: For a 32-year-old woman presenting with narrow-complex tachycardia and stable vital signs but with a significantly elevated heart rate, the immediate goal is to slow the heart rate. The correct choice is (C) Adenosine 6 mg IV. Adenosine is the first-line treatment for stable narrow-complex tachycardias, particularly supraventricular tachycardia (SVT), which is likely in this clinical scenario.
Choice (A), Bretylium, is inappropriate as it is not a first-line agent and is rarely used today due to its side effect profile. Choice (B), Verapamil, is an alternative to adenosine but is generally reserved for cases where adenosine is ineffective or contraindicated. Choice (D), Digoxin, is not typically used in the acute setting of SVT due to its slower onset of action. Lastly, choice (E), Lidocaine, is primarily used for ventricular arrhythmias and would not be the first choice for narrow-complex tachycardia.
A 56-year-old man seeks medical attention due to experiencing nocturnal sweating, unintended weight loss, coughing, and breathlessness. Laboratory analysis reveals blood in his urine. He had a reactive PPD test half a year prior but did not receive treatment. What lung pathology location is likely to be evident on his chest radiograph?
A. Anterior bases of the lungs
B. Left lingula
C. Right middle lobe
D. Posterior bases of the lungs
E. Lung apices
Critique: In the case of a 56-year-old male with night sweats, weight loss, cough, shortness of breath, hematuria, and a past positive PPD skin test, the clinical suspicion of tuberculosis (TB) is high. TB characteristically affects the upper lobes of the lungs, making the correct answer (E) Lung apices.
Choices (A) and (D), the anterior and posterior aspects of the lung bases, are less common for primary TB, which typically presents in the upper lobes due to the higher oxygen concentration favorable for mycobacterial growth. Choice (B), the lingula of the left lung, and choice (C), the right middle lobe, are also less common locations for primary TB.
A nine-year-old boy is brought to your clinic after a snakebite, with the culprit snake in tow. Which characteristic, if observed on the snake, would most strongly suggest the snake is venomous?
A. Pupil shape being elliptical
B. A round-shaped head
C. Two rows of scales beneath the tail
D. The snake’s length
E. A red band adjacent to a black band
Critique: For identifying venomous snakes, the correct choice is (A) Pupil shape being elliptical. Most venomous snakes, particularly pit vipers, have elliptical pupils, much like a cat’s eye.
Choice (B), a round-shaped head, is common in non-venomous snakes, although some venomous snakes can have this feature as well. Choice (C), a double row of caudal plates, is typical of non-venomous snakes. Choice (D), the snake’s length, does not reliably indicate whether a snake is venomous. Choice (E), the presence of a black band next to a red band, is a characteristic of some venomous snakes like the coral snake, but the color pattern alone without the context of geographic location can be misleading due to the presence of mimic species that are non-venomous.
Among the following vaccines, which one is known to prevent a form of cancer?
A. Rubella vaccine
B. Rubeola vaccine
C. Hepatitis B vaccine
D. Influenza vaccine
E. Tetanus vaccine
Critique: The correct choice is (C) Hepatitis B vaccine. The Hepatitis B vaccine prevents Hepatitis B virus infection, which can lead to chronic liver disease and hepatocellular carcinoma, a type of liver cancer.
Choices (A) Rubella vaccine and (B) Rubeola vaccine protect against viral diseases that do not directly cause cancer. Choice (D) Influenza vaccine prevents influenza but has no role in cancer prevention. Choice (E) Tetanus vaccine protects against tetanus and also does not have a role in cancer prevention.
A long-term smoker, a 51-year-old man, reports a chronic cough. His recent chest X-ray does not show any abnormalities. The cough commenced shortly after initiating a new medication. Which drug might be responsible for inducing his cough?
A. Verapamil
B. Digoxin
C. Captopril
D. Acetaminophen
E. Lovastatin
Critique: The likely medication causing the chronic cough in this patient is (C) Captopril. Cough is a well-known side effect of angiotensin-converting enzyme (ACE) inhibitors like captopril due to the accumulation of bradykinin.
Choice (A), Verapamil, and choice (B), Digoxin, are more likely to cause constipation and other cardiac side effects than a cough. Choice (D), Acetaminophen, is not associated with cough. Choice (E), Lovastatin, could cause muscle aches or liver issues but not typically a cough.
Which of the following factors is linked to a lower incidence of ovarian cancer?
A. Having the first child after the age of 40
B. A family history positive for ovarian cancer
C. Age over 50 years
D. Never having been pregnant
E. Use of oral contraceptives
Critique: The factor associated with a reduced risk of ovarian cancer is (E) Use of oral contraceptives. Epidemiological studies have shown that the use of oral contraceptives can significantly reduce the risk of ovarian cancer, likely due to the reduction in ovulation frequency.
Choice (A), delivering the first child after the age of 40, does not decrease the risk; in fact, a later age at first birth can be a risk factor for certain types of ovarian cancer. Choice (B), a positive family history of ovarian cancer, increases risk, not decreases it. Choice (C), present age greater than 50 years old, is another risk factor for ovarian cancer. Choice (D), never having been pregnant, also increases the risk rather than decreasing it.
A patient receives a novel treatment for an acute migraine attack but soon after complains of marked chest constriction. Which medication is likely to have been administered?
A. Promethazine
B. Metoclopramide
C. Sumatriptan
D. Trimethobenzamide
E. Ketorolac
Critique: The correct answer is (C) Sumatriptan. Sumatriptan, a serotonin agonist used to treat acute migraine attacks, can cause chest symptoms due to its vasoconstrictive effects.
Choices (A) Promethazine and (B) Metoclopramide are antiemetics that can be used to treat nausea associated with migraine but are not known to cause chest constriction. Choice (D), Trimethobenzamide, is another antiemetic and also does not typically cause chest constriction. Choice (E), Ketorolac, is a nonsteroidal anti-inflammatory drug used for pain relief and would not usually cause chest constriction as a side effect.
Which of the following is NOT typically a contributing factor to an increased risk of infections in a patient with cancer?
A. Low platelet count
B. Undernutrition
C. Use of therapeutic catheters or shunts
D. Low neutrophil count
E. Removal of the spleen
Critique: The factor that is NOT typically associated with an increased risk of infection in cancer patients is (A) Low platelet count. While a low platelet count increases the risk of bleeding, it does not in itself lead to an increased risk of infection.
Choice (B), Undernutrition, compromises immune function and can increase the risk of infection. Choice (C), the use of therapeutic catheters or shunts, creates a potential entry point for pathogens, thereby increasing infection risk. Choice (D), a low neutrophil count (neutropenia), is directly associated with an increased risk of infection. Choice (E), splenectomy or removal of the spleen, increases the risk of infection, particularly from encapsulated organisms.
A 24-year-old male with a diagnosis of HIV has started treatment with trimethoprim-sulfamethoxazole. He now presents with escalating fatigue and shortness of breath over a period of two days. On examination, he is notably pale and exhibits yellowing of the whites of his eyes. Blood tests reveal significant anemia and a rise in both total and indirect bilirubin levels. Which condition is most consistent with these findings?
A. Crigler-Najjar syndrome
B. Gilbert’s syndrome
C. Glucose-6-phosphate dehydrogenase deficiency
D. Immune reconstitution syndrome
Critique: The presenting symptoms and laboratory findings are most indicative of (C) Glucose-6-phosphate dehydrogenase deficiency. This genetic disorder leads to a defect in an enzyme that protects red blood cells from oxidative damage. Individuals with this condition can experience hemolytic anemia when exposed to certain triggers, such as sulfonamide antibiotics, which the patient recently started. The clinical signs of worsening fatigue, dyspnea, pallor, and scleral icterus, along with the lab results showing anemia and elevated bilirubin, fit the typical profile of hemolytic anemia secondary to G6PD deficiency upon exposure to an oxidative agent.
Condition (A), Crigler-Najjar syndrome, manifests early in life with significant jaundice due to a failure in bilirubin conjugation, leading to high levels of unconjugated bilirubin. Gilbert’s syndrome (B), a more benign hereditary liver disorder, is characterized by occasional, mild elevations of unconjugated bilirubin, usually without anemia. Lastly, Immune reconstitution syndrome (D) refers to a paradoxical worsening of clinical status after commencing antiretroviral therapy for HIV due to the restoration of immune function, which then mounts an inflammatory response against a range of previously subclinical infections; this would not typically present with hemolytic anemia or isolated elevated bilirubin.
A young child presents to the clinic with symptoms of fever, abdominal pain, and muscle aches, in addition to a distinctive rash that spread soon after a tick bite. The lab findings show a decrease in platelets. What treatment should be administered?
A. Amoxicillin
B. Chloramphenicol
C. Dicloxacillin
D. Doxycycline
Critique: Correct Answer: D. Doxycycline
The clinical signs are indicative of Rocky Mountain spotted fever (RMSF), a serious tick-borne illness caused by Rickettsia rickettsii. This disease is prevalent across various regions in America, with higher incidences reported in children and individuals with frequent exposure to environments where ticks thrive. The classic symptom triad includes fever, rash, and a history of a tick bite, with the rash often extending to the palms and soles. The presence of thrombocytopenia and normal white cell count further supports this diagnosis. RMSF can be fatal if not treated promptly; hence, empirical therapy should commence without delay, especially in symptomatic individuals with a suggestive history and clinical presentation.
Doxycycline is the recommended first-line treatment for RMSF across all age groups. The potential risk of dental staining in children is secondary to the urgency of treating this potentially lethal infection.
Choice (A), Amoxicillin, is not effective against the rickettsial organisms responsible for RMSF. Similarly, choice (C), Dicloxacillin, is also ineffective against these intracellular pathogens and is not recommended. Although Chloramphenicol, choice (B), can be used in situations where doxycycline is contraindicated, it is less preferred due to its adverse effect profile and the challenges associated with its usage. Therefore, doxycycline remains the best therapeutic choice to address RMSF and mitigate the high mortality associated with untreated cases.
A 32-year-old female is experiencing rapid heartbeat, palpitations, along with nausea, vomiting, and a high fever. Her medical history reveals a recent diagnosis of Graves' disease. On physical examination, she is sweating profusely, appears restless, and her vitals are as follows: heart rate of 132 bpm, blood pressure at 189/91 mm Hg, and body temperature at 39.4°C. What sequence of therapeutic interventions should be administered for this patient?
A. Hydrocortisone, iodide, propylthiouracil, propranolol
B. Iodide, propranolol, propylthiouracil, hydrocortisone
C. Propranolol, propylthiouracil, iodide, hydrocortisone
D. Propylthiouracil, hydrocortisone, propranolol, iodide
Critique: The woman’s clinical presentation is indicative of a severe hyperthyroid crisis, often referred to as a thyroid storm, which requires prompt and strategic treatment to stabilize her condition. The ideal treatment progression begins with a beta-blocker to rapidly control the symptoms of heightened sympathetic activity, such as rapid heart rate and palpitations. Propranolol is the preferred choice here due to its additional property of blocking the conversion of thyroxine (T4) to the more active triiodothyronine (T3).
Following the initial stabilization, an antithyroid agent like propylthiouracil (PTU) is essential for inhibiting further synthesis of thyroid hormones and also for its added benefit of preventing peripheral conversion of T4 to T3. Iodide administration comes after antithyroid drugs to prevent the thyroid gland from releasing its hormones. Giving iodide before antithyroid drugs could inadvertently fuel the thyroid storm by boosting hormone production. Lastly, hydrocortisone serves to address the potential adrenal insufficiency that can occur with a thyroid storm and aids in suppressing T4 to T3 conversion.
In light of the above, the correct treatment order, which reflects the most effective and safe approach to managing this critical situation, is as follows: Beta-blocker to address the hyperadrenergic state, antithyroid drug to stop hormone synthesis, iodide to block hormone release, and corticosteroid to manage peripheral effects and potential adrenal insufficiency. Thus, the most suitable option is C: Propranolol, followed by propylthiouracil, then iodide, and finally hydrocortisone.
PA School Map Your Guide to Physician Assistant Programs
This comprehensive guide provides everything you need to know about PA school admissions, from choosing the right programs to submitting a competitive application. Learn about the different types of PA programs, the admissions requirements, and how to make the most of your application materials.
How Medical School Admission Consulting Can Help You Stand Out and Succeed
Medical school admissions consulting can help you navigate the complex and competitive admissions process. Experienced consultants can help you develop a strong personal statement, write effective secondary essays, and prepare for your interviews.
International Medical Aid offers a variety of resources to help you prepare for PA school admissions, including a comprehensive guide to PA programs and medical school admissions consulting services. With our help, you can stand out from the competition and increase your chances of getting accepted to your dream school.
Frequently Asked Questions
How often can I take the PANCE?
You can schedule the PANCE according to the available dates, with limits on the number of retakes and mandatory waiting periods between attempts.
What is included in the PANCE blueprint?
The PANCE blueprint outlines the domains of knowledge that the exam covers, which are crucial for the competent practice of a PA-C.
Where can I find resources for PANCE prep?
The NCCPA offers practice exams and various other resources align with the PANCE blueprint and topic list.
What is the cost of the PANCE?
The PANCE cost varies over time, so it’s essential to check the current fee structure and include it in your financial planning.
How should I plan my study schedule for the PANCE?
Your PANCE schedule should include regular study periods, practice exams, and reviews of the PANCE blueprint to ensure a comprehensive preparation strategy.
Professional Competencies for Physician Assistants
Physician assistants must demonstrate a broad range of competencies throughout their careers. These competencies extend from knowledge for practice to societal and population health. The PANCE tests these competencies, ensuring that PAs maintain a standard of care that benefits both individual patients and the broader community. Lifelong learning and adherence to these competencies are fundamental to the PA profession, as outlined in the professional guidelines.
Understanding these competencies, staying informed of PANCE exam dates 2025, preparing with the NCCPA practice exam, and aligning studies with the PANCE blueprint and topic list are crucial steps towards achieving the PA-C designation. Furthermore, experience through Physician Assistant internships abroad and direct patient care hours are practical extensions of these competencies. The physician assistant examination is more than a test. This is a comprehensive evaluation of a candidate’s readiness to contribute to healthcare effectively.
The competencies for the Physician Assistant (PA) profession are defined as the knowledge, skills, and attitudes that PAs should demonstrate throughout their careers, regardless of their clinical specialty or setting within the United States. They are designed to guide PAs in their professional development and to promote the maintenance of their competencies throughout their careers. These competencies are as follows:
Knowledge for Practice
This competency revolves around the PA’s understanding and application of biomedical and clinical sciences to patient care. It includes the ability to critically think and investigate clinical situations, interpret medical information, apply epidemiological principles, discern different disease states, use evidence-based practice skills, adhere to standards of care, allocate healthcare resources effectively, and use technology to improve healthcare access and quality.
Interpersonal and Communication Skills
PAs must demonstrate the ability to effectively communicate and collaborate with patients, their families, and other healthcare professionals. This includes establishing therapeutic relationships, providing culturally competent care, effectively exchanging information, documenting medical information accurately, handling sensitive conversations compassionately, and overcoming communication barriers.
Person-centered Care
This competency is about providing care that is respectful of and responsive to individual patient preferences, needs, and values. It involves gathering essential patient information, interpreting patient data, making informed decisions, developing patient management plans, maintaining proficiency in essential procedures, educating patients, ensuring continuity of care, and preventing health problems.
Interprofessional Collaboration
This domain focuses on the PA’s ability to engage with other health professionals to provide safe, effective, and patient-centered care. This includes working in a respectful manner with a team, enhancing team dynamics, using the expertise of various professionals, collaborating on public health interventions, and referring patients appropriately.
Professionalism and Ethics
PAs should commit to ethical practice and professional behavior. This encompasses adhering to standards of care, showing compassion and respect, being responsive to patients’ needs, demonstrating cultural humility, adhering to ethical business practices, engaging in lifelong learning, promoting personal wellness, and being fiscally responsible.
Practice-based Learning and Quality Improvement
PAs should continuously engage in self-evaluation and practice improvement by critically analyzing their own practice experience, the medical literature, and other information resources. This involves identifying personal knowledge and skill gaps, adopting new knowledge that improves outcomes, using performance data for improvement, and understanding the financial impact of practice decisions.
Society and Population Health
Recognizing the broader determinants of health is key in this competency. PAs should integrate knowledge of these determinants into patient care, which includes assessing the impact of psychosocial and cultural influences on health, recognizing the role of genetic and environmental factors, improving population health, and leading efforts to remove barriers to health.
Each of these competencies outlines a critical area in which PAs are expected to develop and demonstrate proficiency. They are meant to encompass the complexity of modern PA practice and reflect a growing need for medical professionals to be adaptable, knowledgeable, and responsive to the changing healthcare landscape.
IMA Adventure Consulting
Begin an unforgettable expedition with IMA Adventure Consulting, where physician assistant and pre-PA interns amplify their study abroad experience with an exclusive adventure retreat. With IMA Safaris, interns can dive into the splendor and cultural richness of their host country. Leveraging strong connections with reputable guides, accommodation, and travel entities, IMA eases the travel process for interns while providing a consistent line of communication to their families, ensuring tranquility of mind.
Interns will have the pleasure of encountering globally acclaimed attractions and diverse ecosystems. Imagine traversing the storied landscapes of the Masai Mara Game Reserve, ascending the towering heights of Mount Kilimanjaro, witnessing the awe-inspiring cascade of Victoria Falls, discovering the singular wildlife of the Galápagos Islands, exploring the ancient mysteries of Machu Picchu, and roaming the vast plains of the Serengeti National Park. These locales offer more than just a visit—they are canvases for experiences that enrich the interns’ academic and personal narratives.
Good Luck!
As you navigate the path toward becoming a Physician Assistant (PA), the PANCE stands as a crucial milestone, assessing your readiness to enter the field as a certified professional. With an understanding of “how many questions are on the PANCE,” you know to prepare for the 300 questions that will challenge your medical knowledge. Recognizing “how long is the PANCE” equips you with the ability to manage your time effectively during this five-hour examination.
This physician assistant examination is more than a test; it’s a comprehensive evaluation of the critical skills and knowledge you’ve cultivated throughout your education. By adhering to the PANCE schedule, you can structure your studies and ensure you’re well-prepared for the exam day. Moreover, consider the enriching experience of Physician Assistant Internships Abroad, which can offer a broader perspective on healthcare and enhance your clinical acumen.
As you draw closer to the date of your examination, remember that the journey through PA school and internships has been a preparation not just for the PANCE but for a rewarding career ahead. Good luck, and may your dedication to the profession be reflected in your success on the exam and beyond.






