This spring, as we were experiencing lifting of the pandemic restrictions and relishing in the gradual return of normal life, the SARS-CoV-2, B.1.617.2, “Delta” variant was grabbing hold and spreading. First detected in the UK in the Spring of 2021, the Delta variant traced back to India where the mutation was known and spreading months earlier in December 2020.
Delta is not the only coronavirus mutation, but because of it’s menacing characteristics, it is the one to know about. With Delta here, we enter a new phase in the pandemic. This phase seems to resemble a phase we knew nearly a year-and-a-half ago: we don’t know what we don’t know and we hope a vaccine will help.
Scientists say the Delta variant is a dominant form of the coronavirus that is more transmissible and evades immune system response making it more dangerous than the initial “Wuhan” strain.
What is “Variant” About Delta?
Mutations in Delta revolve around protein and their building blocks, amino acids, which ultimately enhance human cell invasion capabilities by the virus. A few Delta mutations we do know about are (1) the Delta variant gene mutation encodes surface spike protein enabling human cell invasion, (2) amino acid mutations enhance protein cutting at cleavage sites, and (3) deleterious mutations resulting in impedance of human immunity against the virus all of which result in increased transmission speed of the virus. The Delta variant also contains numerous mutations we do not know much about. Scientists are transparent that very little is known, and they hope to make progress on Delta in the coming months.
Delta and Vaccines
Due to the Delta variant characteristics, it is hard to slow it, even with the vaccines. Despite the lack of a full understanding of vaccine efficacy against Delta, people are hopeful current vaccinations can and will protect against the Delta variant slowing the outbreak, however Delta has showed signs of partial vaccine resistance. Studies and anecdotal evidence suggest vaccines are slightly less effective against the Delta variant than the original strain or Alpha variant and vaccinated people may still become infected by Delta but may experience less severe symptoms than unvaccinated people. Research shows people who are fully vaccinated are at reduced risk of hospitalization and death related to Delta and are at reduced risk of becoming infected by Delta, but full vaccination is less effective against Delta than it is against other coronavirus strains.
The highest spread, most localized outbreaks, and severe outcomes related to the Delta variant are occurring among unvaccinated people and in low vaccinated areas. Virologists predict Delta outbreaks in low vaccinated areas and Delta boosters are under development, so the vaccine does play a huge role with Delta.
Brace for Impact
With its unique mutations—amino acid and protein changes resulting in high transmission speed and reduced immune resistance—evolutionary biologists predict the Delta variant will usurp as the dominant form of coronavirus worldwide. Compared with the initial strain, Delta is estimated to be 50- to 100-percent more transmissible. As Delta wreaks havoc across the globe, virologists have learned dangerous coronavirus variants cannot be identified quick enough to stop the spread, so the goal becomes limiting further evolution of the virus.
In a CDC document obtained by The New York Times, Delta was described as more transmissible than a cold, influenza, and viruses that cause Ebola, MERS, smallpox, and SARS and dubbed as contagious as chickenpox.
The Delta Variant is Prevalent
The CDC continues to track COVID-19 variants along with vaccine, diagnostic, and treatment implications in the United States. Monitoring emerging variants and spread relies on laboratory based rapid sequencing of the virus. As COVID-19 samples are continuously sequenced and surveilled, corona virus sequences containing similar genetic mutations are grouped into viral lineages.
The proportion of variant lineages in the Unites States can be characterized as variants of high consequence, variants of concern, or variants of interest. The idea is, should a highly consequential variant evolve in the United States, the issue can be contained preventing international spread of the virus before it is identified. With proactive prevention efforts, there is hope we can prevent future phases of the pandemic.
For now, this viral surveillance system is tells us the dominant variant causing coronavirus infections in the U.S. By the end of July, more than 80-percent of all COVID cases in the U.S. were the Delta variant. While still below the height of the pandemic, new cases are surging—more than 140-percent higher 7-day average than earlier in July.
Today, there remains a lot we do not know about the Delta variant. Here are five things we do know, and you should know too.
1. Delta is the Most Contagious Variant
Within months of the Delta variant being identified in India in December 2020, Delta spread to nearly 100 countries becoming a dominant variant in many, including the United States. Now, in the U.S., Delta is causing more than 80-percent of COVID-19 cases. Reports of Delta transmissibility have varied—some say it is 40- to 60-percent more transmissible, while others say 50- to 100-percent more transmissible than initial Wuhan or Alpha variant strains—but all suggest Delta is highly contagious, spreading two to three times faster than earlier strains.
Delta variant patients exhibit significantly more viral particles in the airways with viral loads around 1,000-times higher than other strains. Research shows that Delta enters the respiratory tract then rapidly replicates. The World Health Organization (WHO) deemed Delta the “the fastest and fittest” coronavirus variant to date.
Delta is Fast and Fit for a Reason
Scientists have provided some explanations for the rapid transmission of the Delta variant. Basically, Delta has mutated for optimal human cell invasion.
The Delta covid variant gene mutation encodes a surface spike protein enabling human cell invasion. On the spike protein, there is an N-terminal domain (NTD)—think of an airport terminal, it’s just a region of the structure. The N-terminal domain has 17 amino acids (protein building blocks) that make direct contact with the human cell. The N-terminal domain also has a supersite where all the anti-N-terminal domain antibodies bind. Antibodies are your bodies warriors that fight against antigens which are the virus.
Glycans (sugar molecules) usually shield or camouflage most spike proteins, but the glycans are absent from the N-terminal domain. Furin is an enzyme that cleaves, or removes, sections of a protein after the protein is synthesized so it can be activated. There is a unique spot between the N-terminal domain and another terminal, the C-terminal, where furin cleaves and activates the spike protein.
All strains of coronavirus have spike proteins. Spike proteins in other strains only have one arginine amino acid at the cleavage site between the N and C terminals, but Delta has a mutation at this site that promotes viral spread. In Delta, this furin cleavage site is extended, already cut, and growing at the endoplasmic reticulum—an organelle inside the human cell but outside it’s nucleus—of the infected cell. This furin cleavage causes destabilization, triggering a prefusion state where portions of the N and C terminals swing and oscillate between open and closed states ultimately resulting in confirmational change and the Delta variant infected cell inserting itself into the plasma membrane—outermost barrier—of the human, target cell.
This basic process of mutation in the spike protein results in Delta’s high transmissibility and evasion of immune response scientists call the “immune-evasion phenotype”.
Delta is Primed for Speed
A major characteristic of COVID-19 are the spike proteins protruding from the virus’s surface. The surface spike proteins are covered in glycans (sugar molecules) camouflaging the virus from the human immune system. Hidden in the camouflage is a loop on the spike protein that binds to the human cell receptor.
When the furin enzyme cleaves the mutated amino acid site, the Delta virus is able to enter the lungs with stealth-like efficiency.
Furin cleaving the site is the key to the virus’s ability to rapidly enter the human airway. This is the reason in the beginning of the lifecycle of the Delta virus, immediately following virus assembly, the virus moves into an organelle to be ensconced in furin. The more furin cleaves, the more virus spike proteins are primed to enter human cells. In the Wuhan strain, only 10-percent of spike proteins are primed, in the Delta variant, more than 75-percent of spike proteins are primed.
Furin cleavage sites are also on avian influenza viruses. Furin cleavage in the viral transmission process is not new.
Both the Alpha and Delta variants mutated amino acids at the furin cleavage site to be less acidic and more basic. The more basic (PH), the more effective the furin cleaving process is. This basicity shows us the virus is improving its transmission ability and speed.
Vaccination and Transmissibility
In recent months, 99.5-percent of COVID deaths were among unvaccinated individuals and 97-percent of all current COVID-19 related hospitalizations are unvaccinated patients. Delta is surging in low vaccinated areas, but that doesn’t mean fully vaccinated communities are not at risk.
As people are dismayed over the CDCs recommendation to reimplement mask guidelines, let’s look at an example for why masks are returning despite vaccinations during the Delta phase.
In July 2021, Cape Cod, Massachusetts experienced a Delta variant COVID-19 outbreak, where about 75-percent of the 900 infected people were fully vaccinated. Breakthrough infections by Delta for fully vaccinated people are possible. Research shows that vaccinated people can carry the same amount of virus as unvaccinated people, but much remains unknown. Breakthrough cases continue to be studied. For now, research shows vaccination will reduce hospitalization and death by Delta.
Less than 50-percent of the U.S. population is fully vaccinated.
2. High Risk for the Unvaccinated
Regarding the Delta covid variant, The New England Journal of Medicine published research showing full vaccination effectively prevents COVID-19 related hospitalization and death, however neutralization of the virus is lower against Delta than against the original “Wuhan” coronavirus strain. Though neutralization activity was detected, Delta was 2.9 times less likely to be neutralized by full vaccination than the Wuhan strain.
That said, study findings do suggest that immunity conferred by mRNA vaccines like the Moderna or Pfizer vaccines, will likely hold against Delta.
This research was supported by a study in Nature that showed vaccination resulted in impaired binding at the N-terminal domain (NTD) of the viral spike protein resulting in neutralization of the Delta variant. A third study conducted in the United Kingdom showed full vaccination with mRNA vaccine was 88-percent effective against Delta and partial vaccination was 30.7-percent effective against Delta.
Although less effective at neutralizing the Delta covid variant, research shows full dosage of COVID-19 vaccine can protect against the Delta variant by neutralizing the virus.
Why is Delta so Dangerous for Unvaccinated People?
Unvaccinated people account for more than 95-percent of all COVID-related hospitalizations. The Delta variant boasts unique mutations making it the most infectious variant yet. The virus’s spike protein mutations offer enhanced human cell-binding abilities and when combined with Delta’s covert ability to elude antibodies, our natural ability to neutralize the virus is reduced.
A study showed that unlike the initial strain and other variants, people who catch the Delta covid variant probably become infectious more quickly. The original coronavirus took around six days to detect after infecting a person, whereas Delta is being detected in around four days after infection. This suggests Delta infected people are probably spreading the virus early.
While reports regarding severity and presentation of Delta variant symptomology vary, it is known that Delta has a higher risk of hospitalization than other strains and unvaccinated people with Delta are twice as likely to be hospitalized than unvaccinated people with the Alpha variant. COVID cases and hospitalizations are rising in the U.S. and Delta is surging but it remains unknown whether contracting the Delta variant is a more severe illness. It is known that the majority of COVID-19 related hospitalizations are in low-vaccinated areas and the CDC warns, “this is becoming a pandemic of the unvaccinated.”
3. Spread of COVID Variants in the US
Dr. Wilson, a Yale Medicine Epidemiologist, predicts the transmission rate of the Delta covid variant depends on a regions’ vaccination rate. Dr. Wilson described two different possible scenarios. One is “patchwork vaccination”—areas with high vaccination rates adjacent to areas with low vaccination rates—which easily enables Delta to bounce around within a region. The other is “hyperlocal outbreaks” in unvaccinated areas that are surrounded and contained by highly vaccinated areas where the unvaccinated area turns into an infected hotspot that does not escape more widely in the region.
U.S. Spread
Of all COVID variants in the US, the Delta variant is currently driving the coronavirus spread. The spread of Delta is somewhat reduced by full vaccination. Louisiana State University virologist explained that highly vaccinated areas should be able to thwart the severe ramifications of Delta, like hospitalization and death, but regional and local disparities in vaccination rates may result in severe symptomology and dire outcomes for many. Some areas in the U.S. may experience “localized outbreaks,” such as high proportion Hispanic and African American communities which are exhibiting low vaccination rates and may be highly affected by Delta.
Early research shows the fastest Delta spread is in US counties with a fully vaccinated rate of less than 30-percent. The World Health Organization (WHO) has described four coronavirus variants of concern. Dr. Soumya Swaminathan, WHO, explained Delta is concerning because it is more transmissible and resistant to the natural antibodies in our blood. This means a higher level of antibodies is needed to overcome Delta than other variants. Full vaccination correlates to reduced risk of hospitalization due to the Delta variant. Fully vaccinated people can still contract COVID-19, including Delta, but are at reduced risk of severe symptomology compared to unvaccinated people.
Dr. Walensky of the CDC stated the Delta variant is one of the most infectious respiratory viruses known. According to an internal CDC document obtained by the New York Times, Delta is as transmissible as chickenpox. The Delta variant is driving localized outbreaks in low vaccination rate regions like Arkansas, Missouri, and Nevada. Around 60-percent of adults in the U.S. are fully vaccinated, but vaccination rates have not been even across the country. And of course, children age 10 and under are not vaccine eligible which makes them high risk.
Delta has now been reported in more than 180 countries and is the dominant variant in many, including the US. The good news is with vaccination prevention, experts do not expect coronavirus infections to rise to 2020 peak levels.
4. There is a Lot to Learn About the Delta Variant
We know a little bit about Delta, and we have a lot to learn. Researchers are actively investigating Delta related symptomology, vaccine efficacy, virus structure and function, evolution of the virus, and intelligence of the virus.
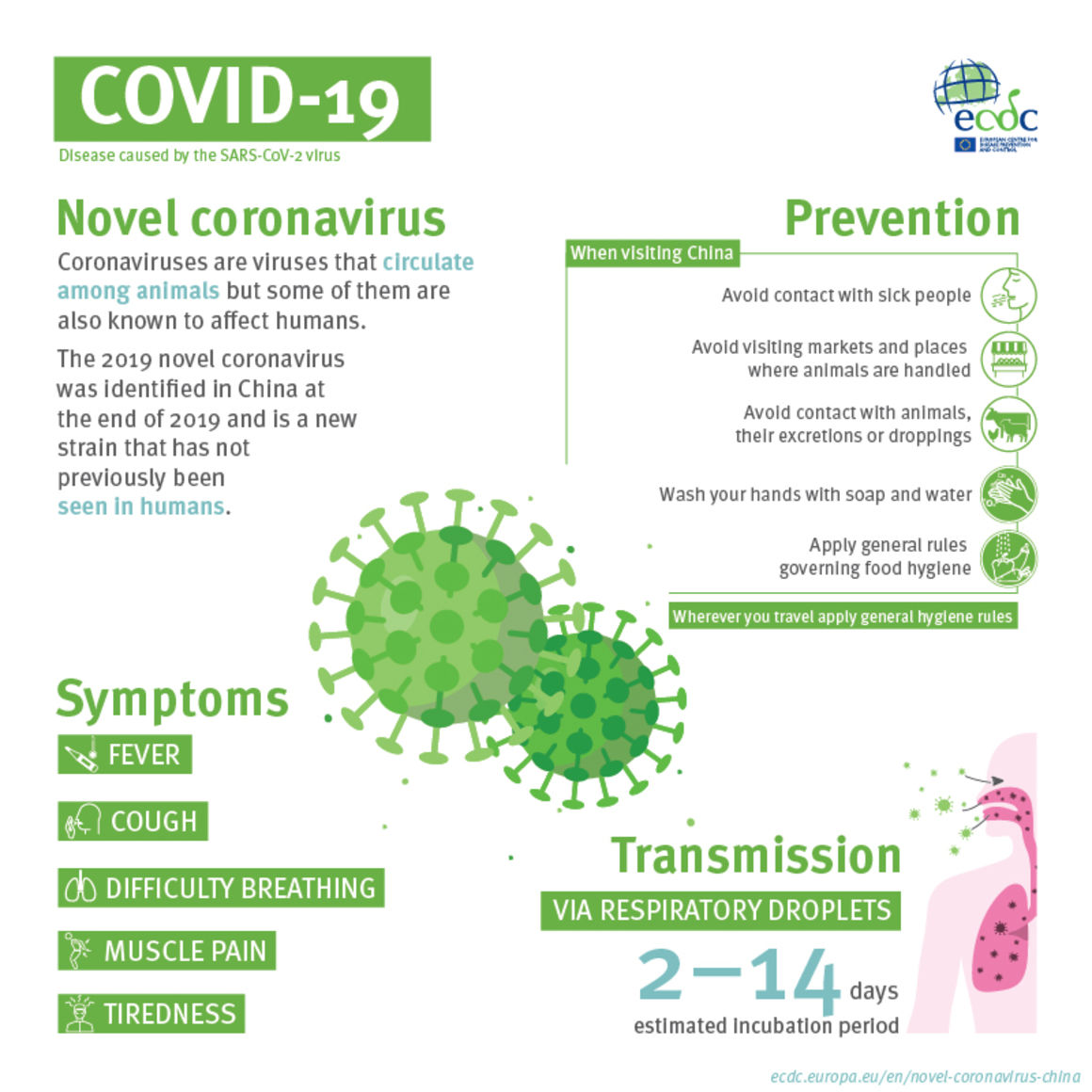
Delta Symptomology
Will the Delta variant make you sicker than other coronavirus strains? Conflicting research exists about the answer to this question. One study in Scotland showed Delta was twice as likely to result in hospitalization, while other studies show there is no significant difference in the severity of symptoms between coronavirus strains. Research also does not definitively tell whether Delta has different or predominant symptoms than other strains. Anecdotal evidence by Dr. Yildirim suggests Delta is associated less with cough and loss of smell and more with the common cold and flu symptoms like fever, runny nose, sore throat, and headache.
The relationship between vaccine efficacy and the Delta variant remains in question, but UK research suggests mRNA vaccines (88-percent efficacy) are nearly 30-percent more effective against the Delta virus symptom onset than non-mRNA vaccines (60-percent efficacy). Ongoing research exists regarding “mix and match” COVID vaccine efficacy.
With Delta wreaking havoc across the world and knowing current vaccinations are less effective against Delta, there has been discussion regarding a Delta booster vaccination. With a possible Delta booster down the road, you may still be asking as things stand, is full vaccination enough protection against the Delta variant? Last month, the Biden Administration did say a third mRNA vaccine may be needed by people with compromised immune systems and/or over the age of 65.
The Virus Itself
Many facets of the Delta variant remain unknown. Unknowns scientists are currently studying include how many ACE2 receptors need to bind to spike proteins, the number of spikes required for fusion between the virus and human cell membranes, and when TMPRSS2 cleaves the S2 (C-Terminal) site.
Virologist David Bauer of the Francis Crick Institute says we remain “in the dark” about the Delta variant. For example, Delta’s nucleocapsid protein has numerous mutations we know nothing about. Further understanding and clarity about Delta will take time.
Most Delta variant mutations currently known about regard transmission efficacy and speed of the virus, not host-cell (human cell) damage. For example, a recent study showed Delta grew more rapidly with a higher viral load in the respiratory system than prior strains.
The Future
Infectious disease and virology experts don’t know how COVID-19 will evolve. We can attempt to predict, but do not know what the future will look like. Dr. Lauring, virologist at University of Michigan Medical School, says anyone who gives a definitive answer about the future of the COVID-19 virus is “full of it.”
Scientists and researchers explain the most important thing right now is to vaccinate as many people as possible because we don’t know how much worse the next variant will be. The experts also say mutations resulting in variants of the coronavirus were completely expected: viruses evolve. Viruses can replicate billions of times in one infected human. With every replication, there is a chance a mutation will occur and change the genetic make up of the virus resulting in altered function, shape, or trait of the virus including transmission traits. For example, with the Delta variant, the mutation resulted in increased transmission speed.
It’s impossible to predict what those changes, or mutations, will look like. Mutations occur in combination with other mutations. A single mutation may not result in a changed trait of the virus, but a pair of mutations or multiple mutations in conjunction may result in a changed trait, like transmission speed. The process and number of possible combinations is too complex to understand or predict. A virus is a profoundly simple organism capable of confounding, complex behaviors.
Lucky for us, general principles about evolution exist, so we know the virus can evolve by three different dimensions: transmissibility (ability of the virus), virulence (symptom severity), or immune escape (ability to evade the human immune system). Although specific mutations of the virus cannot be predicted, we can assume there is an upper limit to the virulence and transmissibility of the virus, and it cannot worsen indefinitely. A computational genomics academic at the National Institute of Health explained the virus will “burn itself out” if it becomes too virulent or transmissible because it will run out of human hosts, or the human immune system will evolve to neutralize it.
The future could look something like other coronaviruses, known as common colds, but we just don’t know. It’s unlikely something entirely new will occur with the pandemic. We generally know how the virus spreads, as each mutated variant is a branch of a known viral lineage.
Race of Intelligence Against the Virus
We do not know what COVID-19 variations are in the future, so scientists continue studying the virus learning everything they can about it. For now, the vaccination is the best chance as preventing the spread, limiting human hosts for the virus, and reducing opportunities for the virus to evolve.
Delta virus structure and function, Delta booster vaccination for stronger Delta neutralization, vaccination efficacy against Delta, Delta symptomology and severity, and many other Delta research efforts are underway. In all this research, we hear a lot about what the viral cell is doing, how it grows in the respiratory system, we hear that our antibodies are affected and eluded by the Delta virus, but we don’t hear a lot about how the rest of the immune system and body is affected and it seems that is because researchers do not know. Research regarding how B and T cells (immune system components) are affected by the vaccine and Delta variant is ongoing.
5. Full Vaccination to Protect Against Delta
Research shows the best way to protect yourself against Delta is to be fully vaccinated where mRNA vaccines currently show the best efficacy against the Delta variant. As the coronavirus continues to mutate and evolve, Dr. Yildirim says, “this is an ongoing risk assessment . . . and the best thing you can do is to get vaccinated.” Studies suggest full dosage of Pfizer, Moderna, and AstraZeneca vaccines are mostly, not completely, effective against the Delta variant.
Breakthrough infections in fully vaccinated people may occur more frequently from the Delta variant, but these infections are usually minor or asymptomatic. Dr. Walensky of the CDC said vaccines were designed to protect against infection and this holds true for Delta with the highest vaccination protection being against severe symptoms, hospitalization, and death. Dr. Peter Hotez, Baylor College of Medicine, suggested fully vaccinated people should do well in the Delta phase of the COVID-19 pandemic—with 88-percent efficacy by the Pfizer vaccine against the Delta variant. However, partial vaccination is only 33-percent effective against Delta and partially vaccinated people should consider themselves high risk.
We know COVID-19 vaccines reduce Delta related hospitalizations and death, but a question of longevity remains: we do not know how long COVID-19 vaccines will offer protection.
How Will You Help?
With method of battling the coronavirus is right for you? When choosing a career in medicine—whether direct patient care as a physician, physician assistant, or nurse or a clinical or laboratory research in medicine—it’s important to comprehensively consider the options from how you will get there to what to expect when you have arrived including educational costs and future earnings. This is a common question with no set answer. The decision is up to you. A Pre-Med Internship or Pre-PA Internship. Will give you deeper insight into the medical field and may help guide your decision. International Medical Aid offers pre-med and pre-PA internships abroad in a variety of disciplines. A well-informed decision about your future awaits you. Explore your options in an immersive and meaningful way to choose the rewarding career you seek.